Sep 14 2015
Is Fibromyalgia Real?
 The question of whether or not fibromyalgia is a real disease is deceptively complex. The answer, therefore, is not a simple yes or no. A thorough answer requires some background, which makes it challenging to discuss any issue related to fibromyalgia without going on a long tangent about its status as a diagnosis.
The question of whether or not fibromyalgia is a real disease is deceptively complex. The answer, therefore, is not a simple yes or no. A thorough answer requires some background, which makes it challenging to discuss any issue related to fibromyalgia without going on a long tangent about its status as a diagnosis.
What’s In a Name?
Before we get to fibromyalgia specifically, I want to review how diagnostic labels are used in medicine. Health care providers, researchers, and also insurance companies and regulators need a common language to refer to what patients have. As our understanding of disease is incomplete, and also disease entities are often complex and fuzzy around the edges, a coherent and thorough diagnostic system is likewise complex.
For simplicity, however, we can divide diagnostic entities into two broad types. First there are discrete diseases, which are pathophysiological entities. This is a specific problem with a specific tissue or physiological process in the body. A disease diagnosis may refer to a specific genetic mutation, for example, or an alteration in a physiological parameter.
A disease diagnosis such as this is often confirmed with specific laboratory findings. This may be so specific that, for example, one particular finding on biopsy equals a specific diagnosis. But of course disease diagnoses exist on a spectrum as well. There may be laboratory markers that are present 60% of the time, or that exist with several diseases. A disease may actually be a category of multiple specific diseases that we have not sorted out yet.
The other type of medical diagnosis can be called a clinical syndrome. Clinical syndromes are defined mostly or entirely by a set of clinical symptoms. Such diagnoses are therefore mostly descriptive. The labels simply recognize that a certain pattern of symptoms tend to cluster together any may have a certain demographic profile or natural history. However, the diagnosis has not yet graduated to a specific disease because we do not understand the underlying pathophysiology.
Historically many clinical syndromes were later discovered to represent a number of specific diseases, and the labels changed as our knowledge changed.
It is imperative, especially for practitioners, to understand the nature of any particular diagnostic label. Is it “real” is too vague a question for many clinical syndromes. They are real in that there are patients who present with the defined set of clinical symptoms, but they may not be real in that they are not a specific pathophysiological entity.
A much better question is whether or not a diagnosis is useful – does it provide any guidance in terms of treatment, prognosis, workup, or research? Some clinical diagnoses are just placeholders for our current ignorance. Others are a useful attempt to capture a real entity and generate hypotheses that can be scientifically tested. Some, such as migraine, are very discrete clinical entities that are perfectly useful as a basis for treatment.
Clinical syndromes are perfectly legitimate, but do create the potential to be misused or even abused. Because they are often vague and rely on non-specific symptoms, without laboratory confirmation, they can easily be used by the lazy or perplexed clinician as a “garbage pail diagnosis.” Everything you don’t understand can be thrown in, just so that you have a label.
We are often forced to use labels, even when we don’t yet understand what is causing the patient’s symptoms. The trick is not to use a label that is more specific than the current understanding of the patient allows.
Fibromyalgia
Fibromyalgia is a controversial clinical diagnosis that suffers from many of these problems as challenges. Here is a description of the diagnosis:
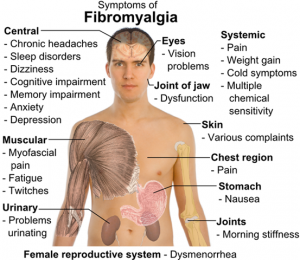
Chronic widespread pain is the hallmark symptom of fibromyalgia and has been proposed to be of neurogenic origin. A central amplified pain perception is linked with allodynia and hyperalgesia. Fatigue and sleep disturbances are also common components of the syndrome. Other key symptoms include tenderness, mood disturbances, and cognitive difficulties. … Anxiety and other mood disorders are common comorbid conditions.
Currently there are no laboratory findings that confirm or exclude the diagnosis of fibromyalgia. It is a clinical diagnosis with a fairly broad description, including many non-specific symptoms, like pain and fatigue. It is also comorbid with other conditions that can potentially cause pain and fatigue, but which in turn can be caused by pain.
This is one of the key challenges of fibromyalgia as a diagnosis – patients with the diagnosis often have a web of interrelated symptoms and it is difficult to impossible to tease apart what is causing what.
When the diagnosis of fibromyalgia was first defined in 1990 it contained as a diagnostic criterion the existence of specific tender points – specific locations on muscles that were tender to the touch. This was really the only specific criterion. Some argue now that this was intended for research purposes, and not for clinical purposes. However, the tender points were frequently ignored. Anyone with diffuse chronic pain and fatigue, with or without specific trigger points, could be given the diagnosis of fibromyalgia.
Interestingly, in response to this common practice, rather than tightening up the use of the fibromyalgia diagnostic label, the American College of Rheumatology simply dropped tender points as a criterion in 2011.
Perhaps the first clue of what might be happening with fibromyalgia is evidence that many patients have what is called central sensitization, or a disorder of pain regulation is which they are more sensitive to pain. What is not known is if this finding is primary or secondary.
In other words, do some patients with fibromyalgia have central sensitization as the primary cause of their symptoms, or is it being caused by some other entity which is the true underlying cause, or is it a result of the chronic pain?
We may need to think of fibromyalgia like fever – it is a physiological process that is a response to many possible underlying causes, but is not a disease unto itself.
For years instead of using the term fibromyalgia I would use other diagnostic labels that I felt were more appropriate, such as myofacial pain syndrome. This label is better, in my opinion, because it focuses on the symptom and describes it as a syndrome. It does not cause confusion by giving the false impression of a specific disease label. However, “fibromyalgia” has essentially come to mean the same thing, especially with the dropping of the specific tender point criterion.
Patients are caught in the middle
Perhaps the biggest problem with the controversy surrounding fibromyalgia as a diagnostic entity is that while scientists and clinicians are debating the utility of this label, how it should be defined and used, there are patients who have chronic pain and other symptoms that need to be treated.
Often times when a patient is given the label of fibromyalgia they take that as validation that their symptoms are real and debilitating. Then when they hear that the diagnosis is questioned, they often take it personally, as if questioning the scientific utility of fibromyalgia as a diagnostic label is an attack on the validation of their symptoms. They interpret questioning the reality of the label as questioning the reality of their symptoms.
This could not be further from the truth, however. Clearly there are many patients who have chronic diffuse pain, fatigue, poor sleep, and other comorbidities. These symptoms often take a great toll on quality of life. Nothing in the scientific discussion about fibromyalgia as a diagnosis calls into question these symptoms. The question is entirely about how we understand the possible cause or causes of these symptoms in order to guide our treatment and research.
One very real risk of using vague diagnostic labels is that they can give the false impression of a specific diagnosis, and therefore end further thinking about possible causes. Settling prematurely on a diagnosis can then result in missing the real underlying cause. Good practitioners don’t let this happen, but it does happen and falsely specific labels encourage this behavior.
Conclusion
Fibromyalgia remains a controversial and poorly understood clinical syndrome. We are in the early stages of understanding what is happening physiologically in patients with this syndrome.
If history is any guide, it is likely that as we tease apart the various underlying causes that are currently lumped under the heading of fibromyalgia, the diagnosis will evolve into many sub-syndromes, and may vanish entirely to be replaced by specific disease diagnoses.






