May 30 2017
Superantibiotic for Superbug
 Imagine a day where you get a bacterial infection, and the doctors tell you that there is no antibiotic which is effective against this bug. It is resistant to everything we have. They can give you supportive care, but the infection just has to run its course and may be fatal. For this reason hospitals have to take extreme measures to prevent the spread of infection – disinfecting and wearing disposable protective garments each time they enter a patient’s room. This is already the case for patients with certain kinds of exposures and infections.
Imagine a day where you get a bacterial infection, and the doctors tell you that there is no antibiotic which is effective against this bug. It is resistant to everything we have. They can give you supportive care, but the infection just has to run its course and may be fatal. For this reason hospitals have to take extreme measures to prevent the spread of infection – disinfecting and wearing disposable protective garments each time they enter a patient’s room. This is already the case for patients with certain kinds of exposures and infections.
This is a serious concern, not hype like most of the doomsday scenarios the press likes to scare you with. Bacteria are slowly (or sometimes not that slowly) evolving resistance to our antibiotics. Even worse, bacteria have loops of DNA called plasmids which they can share with each other. Those plasmids might contain the code for resistance to one or more antibiotics. The more we use antibiotics, the more selective pressure there is for resistance.
The two main things we need to do to avoid a “post-antibiotic era” includes first uses antibiotics as smartly as possible. Use them only when necessary, use narrow-spectrum antibiotics when possible, and complete all courses of antibiotics so all the bacteria are killed.
The second thing we need to do is develop more and better antibiotics. Attacking bacteria using new mechanisms is especially useful. Ideally these antibiotics would be resistant to resistance – they would attack a vulnerability in the bacteria that they cannot easily evolve a defense against.
Even these methods, however, seem like they only delay the inevitable. There are only so many ways to kill a bacterium or stop it from reproducing. Further, they reproduce quickly in vast numbers which means there are lots of opportunities for random mutations to emerge that by chance offer resistance. I do wonder what the really long-term solution will be. Will we have to take certain antibiotics out of use for a few decades to allow resistance to fade? How desperate will the situation get?
My hope is that we will develop new antibiotics and new methods for killing bacteria that are immune to resistance. I am a techno-optimist, but we cannot count on technological breakthroughs. They are unpredictable.
A New Superantibiotic
Scientists are reporting on a new antibiotic, actually a tweaked old antibiotic, which looks promising. This will not be the ultimate solution to the antibiotic resistance problem, but it will buy us some more time if it works. The antibiotic is a modified version of vancomycin. One of the most worrisome “superbugs” is called VRE – vancomycin resistant enterococci.
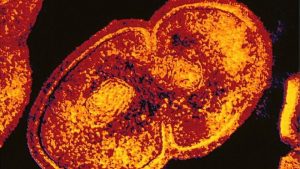
Vancomycin works by inhibiting cell wall synthesis in gram-positive bacteria. In addition it alters cell wall permeability and RNA synthesis. Vancomycin is bacteriocidal, meaning it kills bacteria. Some antibiotics are bacteriostatic, meaning they don’t kill them outright but prevent their reproduction and give the immune system a chance to do its job.
Researchers at Scripps have made three chemical changes to vancomycin to make a deadlier version. The first change makes the primary action of the drug, preventing cell wall synthesis, 1000 times more potent than current vancomycin. This overcomes current resistance to vancomycin.
They also made two changes which add additional mechanisms by which the drug kills bacteria. This is potentially important because it means this one drug will kill certain bacteria by three separate mechanism. This makes it more difficult for bacteria to evolve resistance by chance, because any one bacterium would have to have three beneficial mutations.
When tested against 50 rounds of bacteria, the drug retained “nearly full potency.” While this sounds encouraging, I note it was only “nearly” full. You can ask Nearly Headless Nick from the Harry Potter world how significant the word “nearly” can be.
We know from other experiments, like Richard Lenski’s experiments, that bacteria can evolve traits that require multiple mutations, it just takes longer. So, while this is definitely encouraging, I would not assume that the development of resistance to this triple-mechanism antibiotic cannot emerge, only that it will take longer to emerge. We can avoid resistance by using the antibiotic sparingly and smartly.
The drug so far has only been tested in-vitro. It has not been tested in animals or people. That means we are 5-10 years away from this drug being approved, if it makes it through clinical research. The chemical changes may have also given the drug unwanted properties, and maybe even increased its toxicity to humans, so we have to do the research.
I really hope it works out, though. I also hope that pharmaceutical companies are putting the proper resources into researching new antibiotics. The Scripps approach also seems promising – taking existing antibiotics and tweaking them to make them more potent and overcome resistance. I wonder how much untapped potential there is in this approach.
We are basically in an arms race with bacteria, and they are winning. They are steadily gaining ground on our antibiotics, and we are not researching new drugs fast enough to keep up. While this potential new drug is encouraging, we need to do more.






