Jul 27 2021
Treating Brain Cancer with Magnets
 Magnets for healing have a bad rap, one they rightfully deserve. Magnetic snake-oil devices with all sorts of bogus medical claims are as old as magnets themselves. It may have something to do with the fact that magnets seem like magic, exerting and invisible force at a distance. So it’s often an easy sell. Also, magnets are real and do produce a real energy field (unlike the non-existent “life energy” fields common in alternative medicine). So it makes any claims for them seem all the more plausible.
Magnets for healing have a bad rap, one they rightfully deserve. Magnetic snake-oil devices with all sorts of bogus medical claims are as old as magnets themselves. It may have something to do with the fact that magnets seem like magic, exerting and invisible force at a distance. So it’s often an easy sell. Also, magnets are real and do produce a real energy field (unlike the non-existent “life energy” fields common in alternative medicine). So it makes any claims for them seem all the more plausible.
Because of this, magnets do have real medical applications. Perhaps most common is MRI scans – magnetic resonance imaging. But also there is a lot of research into TMS, transcranial magnetic stimulation, for a variety of neurological indications. Our bodies are electromagnetic devices, and we can alter cell function with electricity and magnetic fields. The trick is, applying them in such a way that they can be exploited for benefit rather than causing harm or having no real effect.
For the consumer with insufficient scientific or medical background, it can be very challenging to tell the difference between a legitimate magnetic medical device and a scam. One good rule of thumb – if the magnet is fairly weak (refrigerator magnet level) it is probably worthless. Real biologically active magnets tend to be powerful. Another slightly more technical fact is that biologically active magnets tend to have an alternating field, while magnetic quack devices tend to have a static magnetic field (which has little biological effect).
Even still, I look at any therapeutic claims about magnets with a huge does of skepticism. Generally I assume it is a scam, or an overenthusiastic researcher, until proven otherwise. But I will look at plausible claims fairly. That is the background and attitude I had when I first saw this report, of a magnetic treatment for a serious brain tumor. A strong word of caution, this in only a case report of a single case. It is premature to get excited about this. Further, even if the claims in the case report are 100% true, this does not necessarily mean that the treatment increases survival. We won’t know that until we have survival data. This is more of a proof of concept, determining that there is enough plausibility here to warrant further research. But the research itself is legitimate as far as it goes.
The treatment is for GBM, glioblastoma multiforme. This is the most common type of brain cancer, also the most aggressive, and has proven remarkably difficult to treat. Survival is 12-18 months on average, and has not improved much even with all of the advances in cancer treatment that have been made over recent decades. This is because the tumor is very invasive. By the time it is detected, it is too late to eradicate it, and any remaining tumor will just grow back and infiltrate more brain tissue. The challenge is also due to the fact that it is in the brain, which limits how aggressively we can go after the tumor. However, this also means that any treatment showing promise needs to be followed up thoroughly. So how does the new treatment allegedly work?
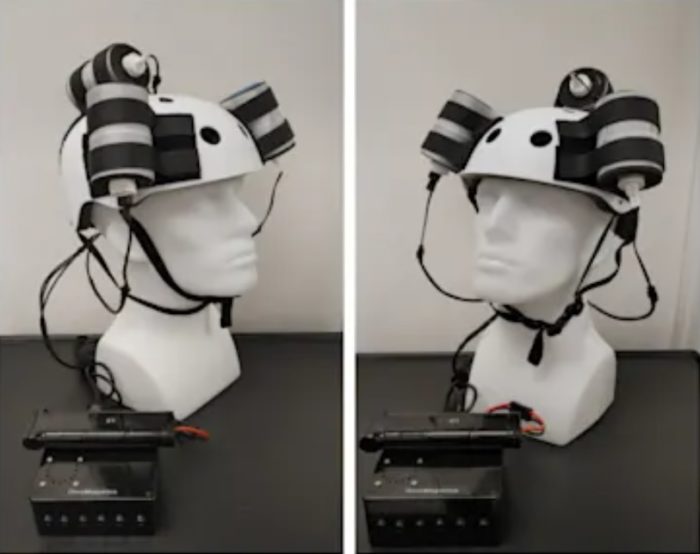
The patient in this case report wore a helmet fixed with three powerful magnets (it kinda looks like a drinking hat, with the magnets being beer-can sized). They produce a powerful alternating magnetic field controlled by an embedded computer. The subject wore the helmet for three hours a day with 5 minute breaks in between each 1 hour session, for give days a week with the weekends off. The idea, based on in vitro studies, is that the powerful alternating magnetic field disrupts the function of mitochondria, the energy producing organelles inside cells. This causes them to produce a much greater amount of oxygen free radicals, which can cause cellular damage. If the concentration of free radicals gets high enough this can trigger apoptosis – cell death. Cancer cells are more metabolically active than healthy cells, so the hope is treatment will have a greater effect on cancer cells, pushing them over the threshold to cell death, without causing significant harm to healthy cells.
The overall result of the treatment was that the tumor shrunk in size by 31%. Here is some more detail:
When the treatment dose was higher (6 hours/day for 4 days) we see a tumor volume reduction rate of 2.32 cm3/day. When it was lower (2 hours/day for 9 days and 3 hours/day for 18 days) the reduction is 1.03 cm3/day. Moreover, when the treatment was paused for 8 days the decreasing trend reversed and the CET volume increased, instead. Assuming that the ~1.03 cm3/day decreasing trend had continued until the treatment was paused, we can estimate that the CET volume grew at the rate of 1.26 cm3/day during the pause. Despite the apparent correlation it is possible that the treatment response is independent of the short-term changes in the treatment dose.
This is an encouraging correlation, even showing a possible dose-response effect. There were no major adverse effects reported, only headaches which seemed to be related to blood pressure and were successfully treated. The treatment is considered non-invasive, and is certainly much safer with fewer side effects than surgery or chemotherapy. Did it improve survival? Unfortunately, we don’t know. The patient had a bad fall (apparently unrelated to treatment) with a closed head injury and eventually died of this injury, so we lost the opportunity to measure survival. But the family did allow for an autopsy to be done, which allowed for the confirmation of the tumor shrinkage by direct pathological assessment.
Again, this is a preliminary study, a case report on a patient who had otherwise exhausted all treatment options and essentially had nothing to lose. It was a demonstration of relative safety and the potential for efficacy. It is enough to justify a larger study, and we will have to wait for that study to see if the treatment really works. It would then need to be determined how this treatment would be incorporated into the standard of care. For example, is this done to shrink the tumor prior to surgery, or to target what is left behind after surgery, or both? Can it be safely combined with chemotherapy? Are there long-term effects on brain health? What is the net effect on quality of life?
There was another unrelated study recently dealing with GBM – using CRISPR to target GBM cells and destroy them by cutting up their DNA. This was done in mice, and will require more safety data before it is tried in humans. But this approach is promising. CRISPR can target the very mutations that make a cell cancerous, and then disable the cell. In the mouse study survival rate was increased by 30%.
Both of these studies are encouraging, but of course we have been here before, and anyone following the GBM research has become at the very least cautious by this point. We have learned to tamp down any premature enthusiasm. But at the least these are two treatments worth following closely.






