Apr 23 2020
Hydroxychloroquine Not Looking Good for Covid-19
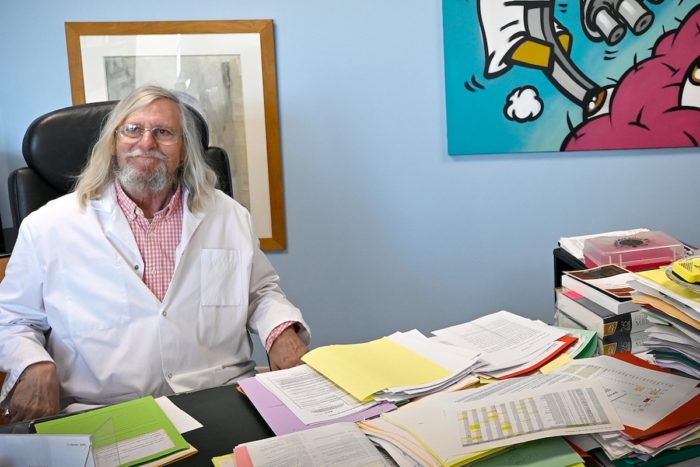 We have been tracking the story of the hype surrounding hydroxychloroquine over at Science-Based Medicine, but there is a brief follow up I wanted to comment on. The short version of the story so far is that one very bad French study claimed to show dramatic reduction in detected virus in those treated. This study, however, was not only preliminary, it was a horrible study, so much so that the results are uninterpretable. The big problem was that it did not count patients who became too sick or died. That is a classic way to make a treatment look better than it is. The author is also a climate change denier who initially mocked China for taking steps to mitigate Covid-19. He does not exactly have street cred within the scientific community.
We have been tracking the story of the hype surrounding hydroxychloroquine over at Science-Based Medicine, but there is a brief follow up I wanted to comment on. The short version of the story so far is that one very bad French study claimed to show dramatic reduction in detected virus in those treated. This study, however, was not only preliminary, it was a horrible study, so much so that the results are uninterpretable. The big problem was that it did not count patients who became too sick or died. That is a classic way to make a treatment look better than it is. The author is also a climate change denier who initially mocked China for taking steps to mitigate Covid-19. He does not exactly have street cred within the scientific community.
But that one horrible study from a sketchy researcher was enough to spark media hype, at least in certain circles, and capture the attention of a president apparently desperate to make this problem go away. Amid the fear of a pandemic, that was a toxic combination. The notion that hydroxychloroquine (with our without the antibiotic, azythromycin) might fight the SARS-Cov2 virus is not implausible. But most things in medicine that are “not implausible” don’t work out. We need high quality clinical science to ultimately tell.
The big question always is – what is the risk vs benefit? Hydroxychloroquine and Azythromycin both have the same potentially deadly side effect, prolonging the QT interval of the heart, which increases the risk for sudden cardiac death. This is a manageable side effect in the right setting, but is potentially serious. This is not a good drug or combination to be taking just on the chance it might help.
The entire episode is a good reason to remind everyone why science-based medicine is so important, the nature of clinical research, and the pitfalls of falling for preliminary data. After that initial terrible study there were two more preliminary studies, the kind that are done to see if there is any potential for the treatment that deserves more rigorous study. An open-label study in China found no benefit from hydroxychloroquine. There was also a French study attempting to replicate the results of the original study, and could not. They also found no benefit from the drug – no reduction in the virus, directly contradicting the original study.
But perhaps most devastating is the most recent study to show results – this was a VA retrospective study comparing patients treated with hydroxychloroquine, hydroxychloroquine + azithromycin, and just usual care. They found no benefit on any measure for those treated with the drugs. However, those treated with the drugs were twice as likely to die:
Rates of death in the HC, HC+AZ, and no HC groups were 27.8%, 22.1%, 11.4%, respectively.
That is a huge red flag, the kind of preliminary finding that could kill the prospects for a new drug. That is exactly the reason that small preliminary studies are done, to make sure the treatment isn’t killing people before doing a larger study. Even these results are not the final word, however. This is a retrospective study, which means subjects were not randomized. It is therefore possible that sicker patients were given the drugs, for example. But we can look at all the preliminary data we have so far and conclude that it’s not looking good for the prospects of hydroxychloroquine as a treatment for Covid-19. Further, this drug has a serious potential side effect that may actually increase the risk of death for those given the treatment.
Certainly, this is not the stage when this drug or combination should be hyped or recommended. It is nothing less than dangerously reckless to do so. Further, hydroxychloroquine is a proven treatment for some autoimmune diseases, like Lupus, and some patients who rely it are finding it difficult to get the drug because demand has spiked due to the hype. It’s pretty much a lose-lose all around.
At this point we do need a double-blind randomized placebo controlled trial of hydroxychloroquine in Covid-19 to get some rigorous evidence. One solid negative trial, however, should end it. If the results are promising, then further study should be done. There would be many finer questions about dose, who should get the drug, who should not get it, etc. But at this point the odds are in favor of this treatment not working out, and in fact being harmful. No one should be taking this drug for Covid-19 outside an approved clinical trial.






