Mar 25 2024
Man Gets Pig Kidney Transplant
 On March 16 surgeons transplanted a kidney taken from a pig into a human recipient, Rick Slayman. So far the transplant is a success, but of course the real test will be how well the kidney functions and for how long. This is the first time such a transplant has been done into a living donor – previous experimental pig transplants were done on brain dead patients.
On March 16 surgeons transplanted a kidney taken from a pig into a human recipient, Rick Slayman. So far the transplant is a success, but of course the real test will be how well the kidney functions and for how long. This is the first time such a transplant has been done into a living donor – previous experimental pig transplants were done on brain dead patients.
This approach to essentially “growing organs” for transplant into humans, in my opinion, has the most potential. There are currently over 100 thousand people on the US transplant waiting list, and many of them will die while waiting. There are not enough organs to go around. If we could somehow manufacture organs, especially ones that have a low risk of immune rejection, that would be a huge medical breakthrough. Currently there are several options.
One is to essentially construct a new organ. Attempts are already underway to 3D print organs from stem cells, which can be taken from the intended recipient. This requires a “scaffold” which is connective tissue taken from an organ where the cells have been stripped off. So you still need, for example, a donor heart. You then strip that heart of cells, 3D print new heart cells onto what’s left to create a new heart. This is tricky technology, and I am not confident it will even work.
Another option is to grow the organs ex-vivo – grow them in a tank of some kind from stem cells taken from the intended recipient. The advantage here is that the organ can potentially be a perfect new organ, entirely human, and with the genetics of the recipient, so no issues with rejection. The main limitation is that it takes time. Considering, however, that people often spend years on the transplant wait list, this could still be an option for some. The problem here is that we don’t currently have the technology to do this.

 I was recently asked what I thought about the Solex AO Scan. The website for the product includes this claim:
I was recently asked what I thought about the Solex AO Scan. The website for the product includes this claim: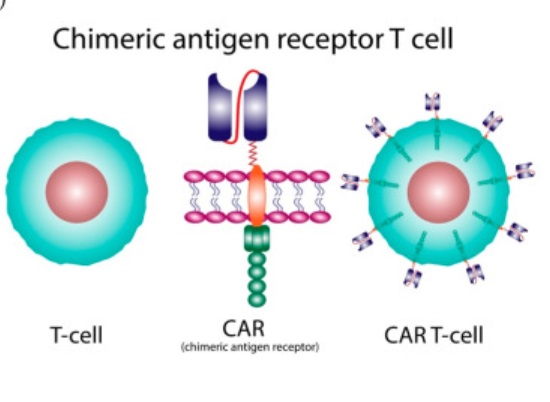 There is a recent medical advance that you may not have heard about unless you are a healthcare professional or encountered it from the patient side – CAR-T cell therapy.
There is a recent medical advance that you may not have heard about unless you are a healthcare professional or encountered it from the patient side – CAR-T cell therapy.  Japan is planning on releasing treated radioactive water from the Fukushima nuclear accident into the ocean. They claim this will be completely safe, but there are
Japan is planning on releasing treated radioactive water from the Fukushima nuclear accident into the ocean. They claim this will be completely safe, but there are 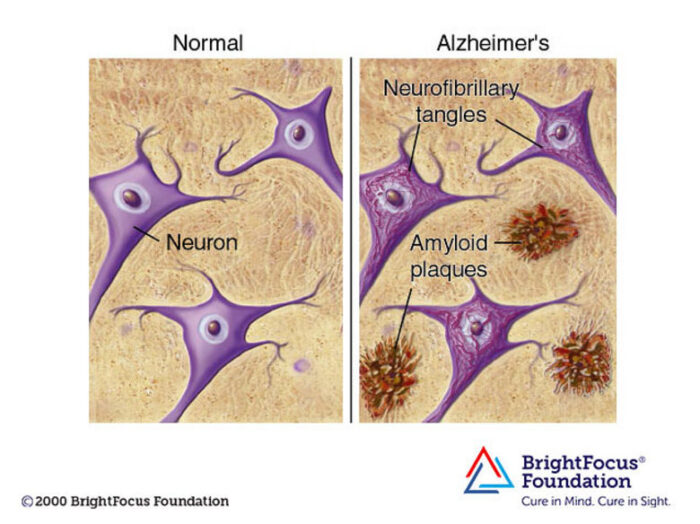 Decades of complex research and persevering through repeated disappointment appears to be finally paying off for the diagnosis and treatment of Alzheimer’s disease (AD). In 2021 Aduhelm was the first drug approved by the FDA (granted contingent accelerated approval) that is potentially disease-modifying in AD. This year
Decades of complex research and persevering through repeated disappointment appears to be finally paying off for the diagnosis and treatment of Alzheimer’s disease (AD). In 2021 Aduhelm was the first drug approved by the FDA (granted contingent accelerated approval) that is potentially disease-modifying in AD. This year Despite robust efforts to fight it, malaria remains one of the most significant infectious diseases affecting humans.
Despite robust efforts to fight it, malaria remains one of the most significant infectious diseases affecting humans. 





