Sep 26 2017
Brain Stimulation in Coma
 The link to the article from the BBC Science News page reads, “Therapy “Wakes” Vegetative-State Patient.” The headline of the article was a bit more conservative, “Vegetative-state patient responds to therapy.” Annoying click-bait aside, what is actually going on here?
The link to the article from the BBC Science News page reads, “Therapy “Wakes” Vegetative-State Patient.” The headline of the article was a bit more conservative, “Vegetative-state patient responds to therapy.” Annoying click-bait aside, what is actually going on here?
Like every such case so far, the improvement in neurological function in this patient with severe coma is extremely limited. This is mostly a proof of concept study, and the results are interesting, but the term “wakes,” even is quotations, is not even close to being justified.
Here is the case report: Restoring consciousness with vagus nerve stimulation. Even that title is a bit misleading – they aren’t saying they actually restored consciousness, just that vagus nerve stimulation might be a viable approach to develop. For background, a vegetative state is one in which basic neurological functions, like breathing, having a sleep-wake cycle, and some automatic movements, are retained. However, the conscious part of the cortex does not appear to be working. By definition there is no reaction to the environment.
By contrast a minimally conscious state has, as the name implies, minimal response to the environment. Patients in this state might blink to threat, or turn to a voice, but cannot communicate or participate in their daily activities. There is a continuum of neurological function from this minimal state to fully conscious.
As I have discussed before, researchers are trying to improve out ability to tell how impaired individual people are who clinically appear to be vegetative or minimally conscious. The challenge is that the neurological exam is limited. If the patient cannot follow commands, we have a limited ability to directly test which circuits in the brain are functioning. The patient may be more conscious than they appear to be because they are paralyzed or deaf, for example. Using functional MRI scanning and EEGs have enhanced our ability to assess brain function in these cases.
There are also researchers trying to find ways to improve the neurological function in these deeply injured patients, with some limited success.
One finding that has come out of this research is that, if a patient appears to be vegetative and they suffered a diffuse anoxic injury (injury to their entire brain due to lack of oxygen), then they probably really are vegetative and their prognosis is essentially zero. If, however, they got to their state from trauma, some of those patients have more brain activity than is apparent by the exam. Some of them may appear vegetative, but with enhanced evaluation are actually minimally conscious.
Further, these minimally conscious patients due to trauma may have hidden neurological function that can be potentially brought out. The best case scenario would be that they still have significant cortical function, but their cortex is asleep because it is not being properly stimulated by the deep structures in the brain. Normally the brainstem and thalamus send stimulating signals to the cortex, producing wakeful consciousness. Without these signals, even an intact cortex would not be able to maintain wakefulness, and the patient would appear comatose.
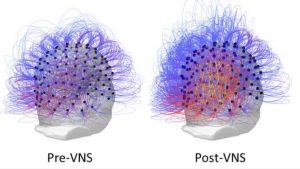
That brings us to the current case. This patient was clinically in a vegetative state for 15 years following a car accident – so they were in that state due to trauma, not diffuse injury. What the researchers did was stimulate their vagus nerve, and through that the thalamus. After a month of this stimulation the patient had a small improvement in clinical function, and an improvement in their EEG activity. They went from a persistent vegetative to a minimally conscious state.
According to the report the patient was able to respond more to the environment, but only minimally. Their eyes would widen when a face approached, for example. They were still not able to communicate or participate in their care.
This one case is a very small step, but it is an important proof of concept. It is consistent with prior research, suggesting that some brain trauma patients may have more neurological function than the exam can demonstrate. Some of these patients, in turn, may be suffering from lack of stimulation to the cortex, and this stimulation can be supplemented artificially.
This is not the first study to do so. Last year researchers reported a similar case, where the thalamus was stimulated by ultrasound waves. Other researchers have implanted stimulating chips into the brain to take over for the thalamus.
One question raised by this recent study is this – how much of the patient’s small improvement was due to direct stimulation and how much was due to actual improvement in brain function through plasticity? In this study it appears the benefits were only present during stimulation, but did seem to improve over time suggesting some plasticity.
These are clearly baby steps. It does, however, suggest that we might be able to get more neurological function out of some brain-injured patients, depending on the exact nature of their injury. While these changes may seem mild, in some patients even a small incremental increase in neurological activity may be significant, if it enables them to interact in any way with their family or participate in their daily activities.
For the future we may be able to optimize this approach with more sophisticated brain-machine interfaces. However, I suspect the benefit will be very limited – wresting a bit of activity out of a damaged brain. Techniques to actually heal some of the brain damage, or functionally replace circuits in the brain, will be needed to get more profound improvement.






