May 14 2024
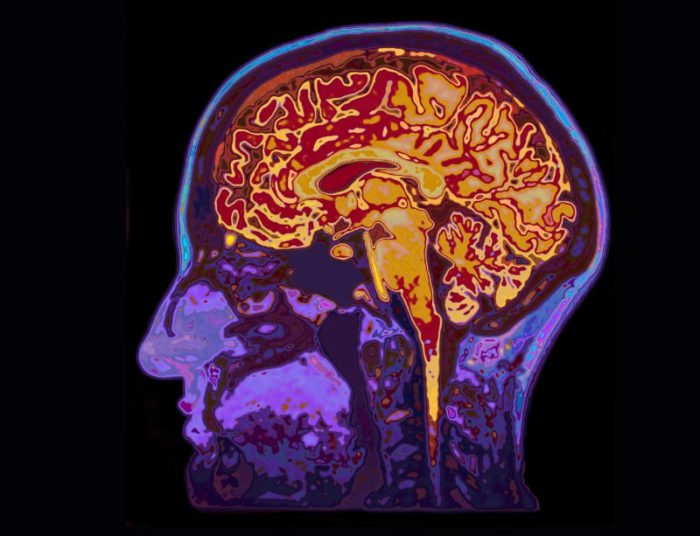
Predicting Outcome in Severe Brain Injury
 One of the most difficult situations that a person can face is to have a loved-one in a critical medical condition and have to make life-or-death medical decisions for them. I have been in this situation many times as the consulting neurologist, and I have seen how weighty this burden can be on family members. Advanced directives are helpful, but they cannot predict every possible situation or anticipate every medical nuance, so still, decisions have to be made.
One of the most difficult situations that a person can face is to have a loved-one in a critical medical condition and have to make life-or-death medical decisions for them. I have been in this situation many times as the consulting neurologist, and I have seen how weighty this burden can be on family members. Advanced directives are helpful, but they cannot predict every possible situation or anticipate every medical nuance, so still, decisions have to be made.
One thing is also clear – the better we are able to predict outcomes, the easier decision-making becomes. Uncertainty is the most difficult aspect of choosing, for example, whether or not to withdraw life-saving interventions. For this reason there has been a lot of research trying to help do exactly that – predict outcomes in various situations of neurological injury, so at least family members can make the most informed decision possible.
But one thing that doctors do not have, as we are fond of saying, is a crystal ball. We cannot say what an individual’s outcome will be, only make statistical statements based on predictive variables. Still, statistics can be extremely helpful.
A recent study adds to the literature addressing this question. They look at the outcomes of 146 adults with severe traumatic brain injury admitted to an ICU. They looked at whether or not there was withdrawal of life-sustaining treatment (WLST) and compared the characteristics of both groups. Not surprisingly, those who were WLST + were older on average and had more severe injury. The researchers also looked at those who were WLST – (did not have withdrawal of life-sustaining treatment) and tracked their outcomes.
First they divided the WLST – cohort into different tiers based upon how likely they were to have treatment withdrawn, with tier 1 and 2 patients being less severe and tier 3 being the most severe injuries. At six months of the 56 WLST – patients, 31 died (55%) but > 30% recovered at least partial independence. Only 3 were considered to be in a persistent vegetative state. Four individuals made a full recovery. Of the tier 3 patients, none had partial independence at 6 months, but some did at 12 months.
They then compared this group to matched subjects in the WLST + group and showed that, statistically, some of the people for whom life support was withdrawn would likely have recovered to at least partial independence. Because of this the authors recommend taking a more cautious approach to prognosticating in the short term after severe traumatic brain injury. This is a reasonable recommendation, but I need to point out some details to put it all into perspective.
First, we must note that this data only applies to traumatic brain injury, not all severe neurological conditions. It has long been known based on prior research that it is more difficult to predict neurological outcomes after traumatic injury compared to other conditions, such as diffuse anoxic ischemic injury. In the later condition, the brain has gone without oxygen for long enough to cause significant damage. We are actually much better at predicting outcome in these cases based upon the neurological exam. The reason is that the damage is diffuse – patients are not responsive because their cortex has been widely damaged. It is very difficult to recovery from this type of injury.
But research has shown that the same data does not apply to traumatic brain injury, and the reason is primarily because the injury is not to the entire brain, but more to some parts than others. This has several implications. First, there may be parts of the cortex, of the thinking part of the brain, that are relatively spared. These spared parts of the brain may eventually allow for significant neurological function after recovery.
Also, patients with more focal brain injury may look a lot worse on exam than they truly are, because focal deficits (like the inability to process sound or vision, or language impairment) may interfere with the patient’s ability to interact with the outside world. They may not follow commands, for example, because they are not processing language, not because they are unable to generate consciousness. This is why, in the current study, patients with spinal cord injury were excluded – because that is another variable that could impair their function but not related to brain injury itself.
Traumatic injury can only involve some reversible pathology, like bleeding. Whenever there is blood in the brain, for prognostic purposes it’s best to wait until the blood is fully resorbed – sometimes the underlying brain tissue is in better shape than it might initially seem.
The same studies that show us we need to be very cautious when making a prognosis in traumatic brain injury also shows that our predictions are pretty accurate in non-traumatic brain injury, such as anoxic damage. This data, therefore, should not be used to argue for uncertainty in such situations. Patients in a persistent vegetative state after a certain amount of time due to diffuse anoxic injury have a very predictably poor outcome. Similarly, this study excluded anyone determined to be brain dead, so the data cannot be extrapolated to that situation.
But if someone is unconscious due to severe traumatic brain injury, especially if they are in the milder end of the spectrum, we should be extremely cautious in making predictions. It may be inappropriate to make decisions about withdrawal of life-sustaining interventions in the first 72 hours or so after such an injury. That is a situation where it may be best to give a patient time to recover.
I say “may” because still there are lots of variables and the decision has to be individualized. At the severe end of the spectrum it gets progressively easier to predict a bad outcome, and the details matter. The pre-traumatic health of the patient also significantly matters. But this additional information is helpful, and consistent with the overall direction of prior research, in highlighting cases in which we need to be more cautious.






