Dec 29 2014
Pertussis Evolving
New evidence suggests that strains of the bacterium, Bordetella pertussis, which is responsible for whooping cough, may be evolving to evade immune protection afforded by the pertussis vaccine.
The research, led by Dr Andrew Preston from the University of Bath, evaluated surface proteins from the 2012 whooping cough outbreak. They found that surface proteins that are included in the acellular pertussis vaccine were evolving faster than surface proteins not included in the vaccine. The authors point out that this was happening even prior to the introduction of the vaccine, but has accelerated since the vaccine.
It is not yet clear what, if anything, this means for the effectiveness of the acellular pertussis vaccine. However, the concern is that circulating strains of B. pertussis will continue to evolve, diminishing the protection provided by existing vaccines.
Whooping cough is a potentially serious illness, primarily affecting infants. There was an outbreak in the UK in 2012 with 10,000 confirmed cases and 14 infant deaths. In the US that same year there were over 48,000 cases reported (not necessarily confirmed) and 20 deaths.
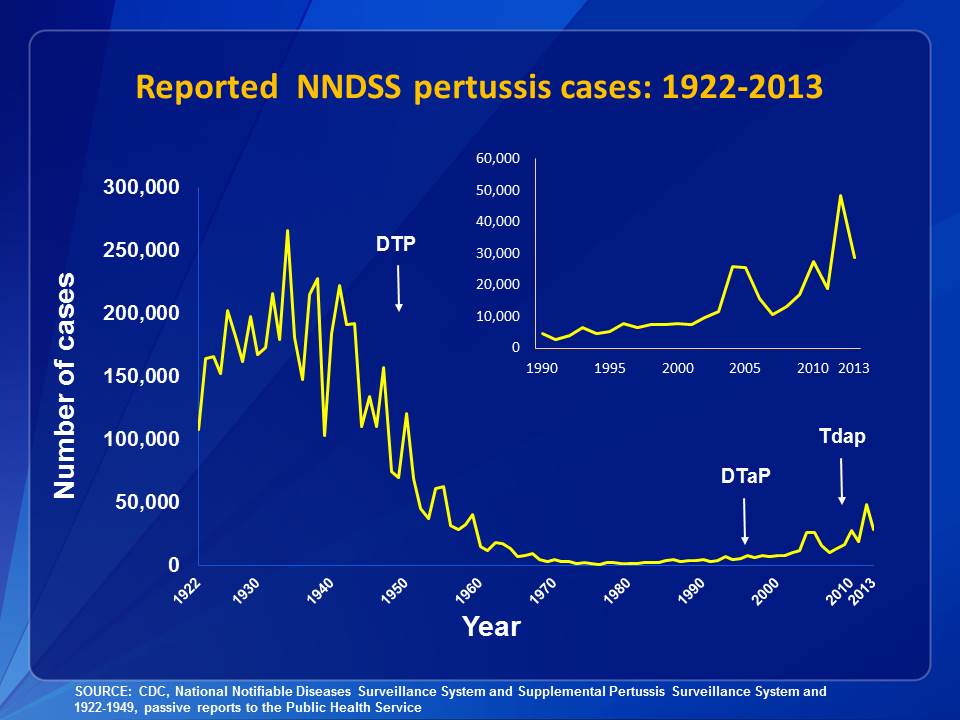
As you can see by the incidence graph from the CDC, whooping cough was a major illness prior to the introduction of the vaccine. With the introduction of the whole cell pertussis vaccine, the incidence plummeted to almost zero. In the last two decades, however, pertussis has been returning, with increasing outbreaks. The exact cause for this is unclear but there are several likely factors.
The most important factor is vaccine compliance. The anti-vaccine movement has created fear around all vaccines, leading to a reduction in herd immunity and a return of previously well controlled infectious diseases, such as whooping cough.
Another possible factor is the switch from the whole cell pertussis vaccine to the acellular vaccine. This switch was made in the 1990s, in response to fears over the safety of the whole cell vaccine. There is no question that the whole cell vaccine in some caused fevers, febrile seizures, and fainting, and the acellular vaccine does not cause these side effects and so has a better safety profile. However, the switch was mainly due to unconfirmed reports of more serious side effects, such as brain damage and death.
Before the science could be sorted out, a media frenzy over possible risks of the whole cell vaccine prompted a switch to the acellular vaccine. The acellular version contains a few target proteins, rather than the whole bacterium. This is generally a safer and more targeted type of vaccine, but it also provides less immunity. Recent studies have confirmed that the acellular pertussis vaccine provides less protection than the older whole cell vaccine.
The question now, of course, is whether the risk vs benefit favors the whole cell vs acellular vaccine, especially given the recent outbreaks and the evolving strains of pertussis. Were the 20 whooping cough infant deaths in 2012 greater than the number of serious side effects that would have occurred from the whole cell vaccine?
The third factor, in addition to non-compliance and the switch to the acellular vaccine, is the evolving strains of pertussis – a factor that is related to the first two. Vaccine non-compliance leads to outbreaks, in which the bacteria has a chance to reproduce at greater numbers, providing the greater opportunity to evolve new strains. The best way to keep a bacteria or virus from evolving resistance is to keep it from reproducing and spreading.
Now we face a dilemma, but there are possible solutions available to us. One option will be to simply develop newer versions of the acellular vaccine that target the new strains, and perhaps target a greater number of proteins. Another option is increased vaccine coverage. Recent research, for example, has found that if pregnant women get their whooping cough boosters, they will pass on immunity to their infants, which can protect them until they are old enough to get the vaccine themselves.
Some researchers are even talking about bringing back the whole cell vaccine. While this might be an effective approach, I doubt this will happen due to public fears.
Conclusion
The whooping cough vaccine (DTaP for those under 7 and TDaP for those 11 and older) is still a safe and effective means of preventing whooping cough (the same vaccine also protects against diptheria and tetanus). There are now some concerns about the pertussis bacterium evolving new strains that will be less well targeted by the current vaccine, but it is not even clear if this is affecting the vaccine’s efficacy.
The current research is an early warning system of a potential problem in the future. Preventing any issues with the pertussis vaccine should be easy enough to achieve with new versions of the vaccine.
This is all part of the ongoing battle with infectious diseases. As we develop new methods to fight infections, the bacteria and viruses will evolve resistance to whatever methods we develop. It is important, however, that we minimize and slow down the evolution of resistance as much as possible.
This is mainly a problem for antibiotics – their overuse, incomplete use, and improper use contribute to bacterial resistance.
Vaccines have very little problem with resistance, because they are preventive. They don’t afford the bugs an opportunity to reproduce extensively, increasing the probability of random mutations leading to resistance. The biggest factors that can lead to vaccine resistance, however, appear to be non-compliance and possibly using very narrow vaccines that target only a few proteins.
One can already argue that it is everyone’s duty to get vaccinated, not only to protect themselves but to contribute to herd immunity for everyone. We can now reasonably argue that this duty extends to minimizing resistance to the existing vaccines. Non-compliance can not only lead to outbreaks, but to diminishing effectiveness of the vaccines for everyone.






