Jun 06 2025
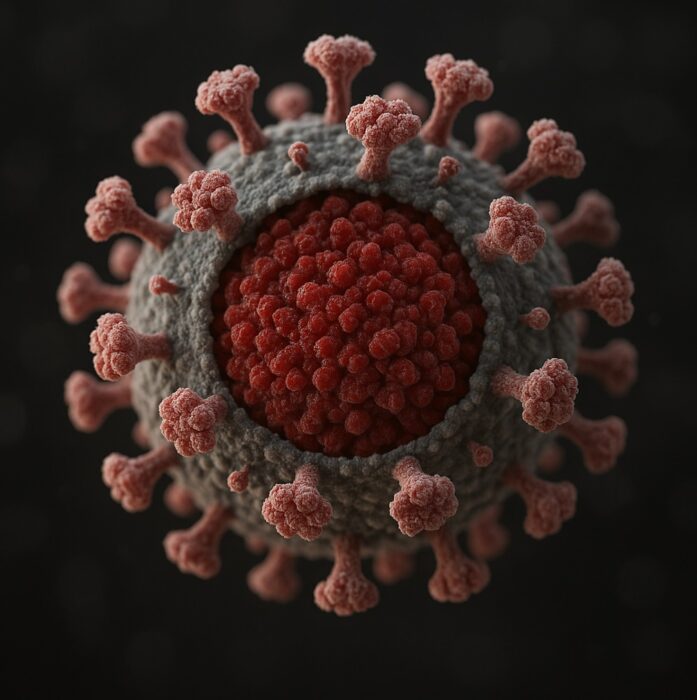
New Potential mRNA HIV Treatment
 First, don’t get too excited, this is a laboratory study, which means if all goes well we are about a decade or more from an actual treatment. The study, however, is a nice demonstration of the potential of recent biotechnology, specifically mRNA technology and lipid nanoparticles. We are seeing some real benefits building on decades of basic science research. It is a hopeful sign of the potential of biotechnology to improve our lives. It is also a painful reminder of how much damage is being done by the current administration’s defunding of that very science and the institutions that make it happen.
First, don’t get too excited, this is a laboratory study, which means if all goes well we are about a decade or more from an actual treatment. The study, however, is a nice demonstration of the potential of recent biotechnology, specifically mRNA technology and lipid nanoparticles. We are seeing some real benefits building on decades of basic science research. It is a hopeful sign of the potential of biotechnology to improve our lives. It is also a painful reminder of how much damage is being done by the current administration’s defunding of that very science and the institutions that make it happen.
The study –Efficient mRNA delivery to resting T cells to reverse HIV latency – is looking for a solution to a particular problem in the treatment of HIV. The virus likes to hide inside white blood cells (CD4+ T cells). There the virus will wait in a latent stage and can activate later. It acts as a reservoir of virus that can keep the infection going, even in the face of effective anti-HIV drugs and immune attack. It is part of what makes HIV so difficult to fully eliminate from the body.
We already have drugs that address this issue. They are called, appropriately, latency-reversing agents (LRAs), and include Romidepsin, Panobinostat, and Vorinostat. These drugs inhibit an enzyme which allows the virus to hide inside white blood cells. So this isn’t a new idea, and there are already effective treatments, which do make other anti-HIV drugs more effective and keep viral counts very low. But they are not quite effective enough to allow for total virus elimination. More and more effective LRAs, therefore, could be highly beneficial to HIV treatment.
This new approach addresses the fact that latent HIV is “transcriptionally silent”, meaning that it is not making HIV proteins from its RNA. Therefore it cannot be detected by the immune system, and it is not engaging in activity that allows anti-HIV drugs to target it. What the researchers did was create a messenger RNA (mRNA) designed to force the viruses into becoming transcriptionally active – forcing them out of the latent stage. This allows them to be targeted by the immune system and anti-HIV drugs.
In order to get the mRNA to the target T cells they encased them in lipid nanoparticles. These are basically tiny fat bubbles that can be engineered to have specific proteins on their membrane which will guide the particles to a particular target and deliver the payload. This is one of those technologies that don’t get a lot of headlines themselves, but they are recently often the tech behind the headlines. The recent case of the personalized CRISPR treatment of the infant with a rare genetic mutation of the carbamoyl phosphate synthetase 1 (CPS1) enzyme is an example. The treatment has apparently worked very well – and not surprisingly the CRISPR payload was delivered by lipid nanoparticles.
In the ex vivo study, using donated T cells from HIV patients, found:
“Encapsulating an mRNA encoding the HIV Tat protein, an activator of HIV transcription, LNP X enhances HIV transcription in ex vivo CD4+ T cells from people living with HIV. LNP X further enables the delivery of clustered regularly interspaced short palindromic repeats (CRISPR) activation machinery to modulate both viral and host gene transcription.”
In other words, it works, at least from a basic science perspective. Next up will be animal studies, then safety human trials and finally human efficacy trials. This will take years, and the treatment may not ultimate work. But it’s very promising. And again, perhaps the most exciting thing about this research is that it further demonstrates the potential of CRISPR, mRNA technology, and lipid nanoparticles. We are transitioning into a new phase of advanced medical technology. But there is, of course, years and even decades of work ahead to make increasing use of these technologies. They are still tricky, and expensive, and need to be tailored to each specific disease, and in some cases specific patients.
KJ’s treatment likely cost about a million dollars to develop (which is similar to the cost of a liver transplant that may now not be necessary), and required the collaboration of about half a dozen institutions. This is happening in the US because of our history of heavily funding biomedical research. Such science funding is an investment, which supercharges our economy and is the secret to America’s dominance as a superpower. Sabotaging this engine of innovation and competitiveness is an incredible self-inflicted wound that will harm American competitiveness for a generation or more.
We may never fully recover. It is creating a brain-drain from the US, and allowing other countries, both allies and enemies alike, to bolster their science and research infrastructure. China is likely to benefit the most. And once those institutions of research are created, they won’t go away just because we try to build back what was lost. This is likely to result in an essentially permanent shift of advantage in science and technology from the US to China and elsewhere. It is an historical advantage that we cannot just recreate. And it’s not just a shift – this will slow the pace of advance for the world. Building institutional knowledge and capability takes decades. It is one of the most reckless things I have ever witnessed, and it’s still hard to grapple with how absolutely insane it is.
This self-destructive policy makes every science news item like this one bittersweet. We are sitting on this stunning biotechnology with the promise of transforming medicine, while we are dismantling the infrastructure that made it all possible.






