Jun 18 2018
Gut Microbiome and Anxiety
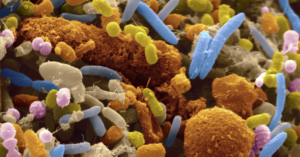 Humans are a symbiotic creature, like pretty much all other animals. It is estimated that there are as many bacteria in your body as there are human cells. Bacterial cells are much smaller, so this amounts to 1-3% of body weight.
Humans are a symbiotic creature, like pretty much all other animals. It is estimated that there are as many bacteria in your body as there are human cells. Bacterial cells are much smaller, so this amounts to 1-3% of body weight.
Bacterial cells line all mucous membranes, where they serve critical functions. They are a critical part of our immune system, crowding out other bacteria and organisms that can potentially cause infection. Many of our bacteria live in the gastrointestinal system, our “gut microbiome” , “microbiota”, or “flora”, where they also aid in digestion.
As is often the case, scientists have been discovering that our relationship with our friendly bacteria is more complex than we thought. The microbiome is not a collection of random bacteria, but a stable ecosystem. There is also evidence that there are only a few distinct types of bacterial ecosystems in people. We have an “enterotype” which may affect our health.
There is also growing evidence that our gut microbiota not only have local effects within our GI system, but may have remote effects on the brain and nervous system. This suggests that some bacteria produce neurotransmitters, hormones, or some chemical signal that can get into the blood and then travel to other parts of the body and have an effect.
Microbiome and Anxiety
A recent study adds to this growing evidence of remote effects for our gut microbiome. The researchers fed mice a high fat diet leading to obesity. They also monitored several behaviors that serve as markers for anxiety and depression in mice, such as compulsive behaviors. They found that the mice fed the high fat diet had increased anxiety and depression.
However, they also fed another group of mice a high fat diet and antibiotics. They also gained weight, but did not develop behaviors indicating anxiety and depression. The effect was almost completely blocked. One interpretation of this result is that changes in the microbiome, changes which were blocked by the antibiotics, caused the anxiety and depression. But there are other possible interpretations, such as a direct effect of the antibiotics.
The researchers also transferred the gut microbiome from the anxious mice fed the high-fat diet to mice fed a normal diet, and they too developed markers for anxiety and depression. Together this evidence strongly suggests a gut microbiome connection to the anxiety.
Of course, the primary limitation of this study, in terms of applicability to humans, is that it was conducted in mice. You cannot ethically do the same study in people. But the researchers may learn about the effect and apply that knowledge to further studies in human. The researchers are now focusing on identifying the molecular signals, which they suspect are neurotransmitters, that are responsible for the observed effect.
The ultimate goal would be to identify the same or a similar microbiome in human subjects with anxiety and/or depression, and then treat their anxiety by changing their microbiome.
Other researchers are exploring other possible remote or biochemical effects resulting from various gut microbiomes or enterotypes. There are links to obesity itself, inflammatory diseases, and (unsurprisingly) GI symptoms like irritable bowel syndrome.
It’s also interesting to note that at least one disease is clearly caused by a GI bacterium – H. pylori causing gastric ulcers, which is successfully treated with antibiotics.
Changing the Microbiome
While all this is extremely interesting and potentially useful, it is turning out to be difficult to permanently change the gut microbiome. Again this is because the microbiome is not a random assortment of bacteria, but a stable ecosystem. There reason there are limited discrete types of microbiomes is likely because there are limited stable assemblages of various bacterial species. The average person has about 100 different bacterial species in their gut microbiome.
Just adding one or a few species of bacteria to the mix does not seem to have any significant effect. This is why probiotic products on the market are largely useless. As Marc Crislip once pointed out, it’s like planting rows of corn in the rainforest – this is unlikely to affect the ecosystem. Probiotics, if given in high enough amounts early on, may be a short term bandaid to help reduce GI symptoms or the emergence of pathogenic bacteria when taking broad spectrum antibiotics. They can act as a placeholder until the normal microbiome has a chance to reestablish itself. But for healthy individuals, probiotics don’t seem to have any benefit, which makes sense.
If we want to shift from one stable microbiome to another, more drastic measures need to be taken. This is why research has been focusing on fecal transplants. Feces are loaded with the entire range of gut bacteria, and therefore can act as a seed to transplant the entire ecosystem, not just a few species. But first you have to clear the way, which can be done with antibiotics.
This is essentially where we are with the science. We are discovering ways in which the microbiome affects health, and working out the basic technology for reconstituting and possibly even changing the microbiome.
But this field is really in its infancy. It is interesting to speculate about where it can go. Obviously we should avoid hype about any new approach being a panacea, and it is easy to get overexcited about the potential of an entirely new field. At first, when a new biological phenomenon is discovered, there is the tendency to implicate the new phenomenon in everything, and therefore think that we are onto a cure for everything. That never pans out, but it may lead to a powerful new way to treat illness.
At this point it seems likely that we eventually will develop effective ways to alter the gut microbiome to help address several issues – including anxiety, obesity, and some inflammatory diseases. But likely these interventions will only be effective in a subset of patients with these disorders.
Perhaps we will discover new stable enterotypes that we can engineer, that may have benefits in terms of reducing risk factors for various diseases or promoting health in other ways. As the microbiome technology advances further, we may be able to genetically engineer bacteria with very specific properties, to optimize health promotion, enhance immune function, or reduce cardiovascular disease. There may even be some designer bacteria for reducing hangovers, eliminating bad breath, reducing the volume and/or offensiveness of flatulence, and other creative effects.
I would love to see where the pinnacle of this technology will lead. We are living in symbiosis with our bacteria – they are (by cell count) 50% of us. From this perspective, we have been ignoring half the cells in our body in terms of health and disease. Let’s see what we can accomplish by focusing on the other half.






