Sep 29 2020
COVID – Not Close to Herd Immunity
 One question weighing on the minds of many people today is – when will this all end? And by “this” (well, one of the “thises”) I mean the pandemic. Experts have been saying all along that we need to buckle up and get read for a long ride on the pandemic express. This is a marathon, and we need to be psychologically prepared for what we are doing now being the new normal for a long time. The big question is – what will it take to end the pandemic?
One question weighing on the minds of many people today is – when will this all end? And by “this” (well, one of the “thises”) I mean the pandemic. Experts have been saying all along that we need to buckle up and get read for a long ride on the pandemic express. This is a marathon, and we need to be psychologically prepared for what we are doing now being the new normal for a long time. The big question is – what will it take to end the pandemic?
Many people are pinning their hopes on a vaccine (or several). This is probably our best chance, and the world-wide effort to quickly develop possible vaccines against SARS-CoV-2 has been impressive. There are currently 11 vaccines in late stage Phase 3 clinical trials. There are also 5 vaccines approved for limited early use. No vaccines are yet approved for general use. If all goes well we might expect one or more vaccines to have general approval by the end of the year, which means wide distribution by the end of 2021. That is, if all goes well. This is still new, and we are fast-tracking this vaccine. This is not a bad thing and does not necessarily mean we are rushing it, but it means we won’t know until we know. Scientists need to confirm how much immunity any particular vaccine produces, and how long it lasts. We also need to track them seriously for side effects.
Early on there was much speculation about the pandemic just burning itself out, or being seasonal and so going away in the summer. Neither of these things happened. In fact, the pandemic is giving the virus lots of opportunity to mutate, and a new more contagious strain of the virus has been dominating since July. Pandemics do eventually end, but that’s not the same as them going away. Some viruses just become endemic in the world population, and they come and go over time. We now, for example, just live with the flu, and with HIV. So perhaps COVID will just be one more chronic illness plaguing humanity that we have to deal with.
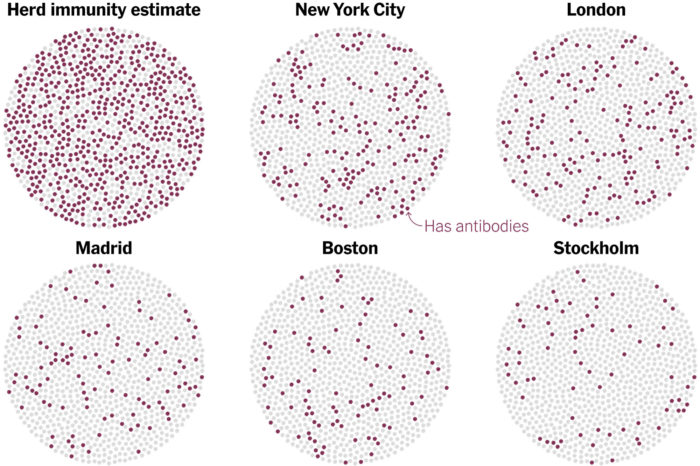
But what about herd immunity? The point of an aggressive vaccine program is to create herd immunity – giving so many people resistance that the virus has difficulty finding susceptible hosts and cannot easily spread. The percent of the population with immunity necessary for this to happen depends on how contagious the infectious agent is, and ranges from about 50-90%. We don’t know yet where COVID-19 falls, but this is a contagious virus so will probably be closer to 90%. One question is, how much immunity is the pandemic itself causing, and will we naturally get to herd immunity, even without a vaccine? The results of a new study suggest the answer is no.
The study is a massive survey of 28,503 Americans in 46 different states. These are all patients on dialysis, and were chosen as a convenience sample because they have their blood drawn on a regular basis. They also are fairly demographically representative of the US as a whole (non-hispanic black was slightly underrepresented). What they found is that, if you standardize to the general population, about 9.3% of people have antibodies to SARS-CoV-2. There were regional differences that follow the density of COVID cases, with the highest percentage being about 25% in the Northeast. This number is about 10 times the number of confirmed COVID cases, so many people are being exposed to the virus without ever being diagnosed (whether or not they develop symptoms).
What does this mean for herd immunity? This means that on average we would need about five times as many cases as we have already had in order to reach the low end of herd immunity, and more likely we would need 8-9 times more cases. We have already had over 200,000 deaths in the US, so that would mean 1-2 million deaths before getting to natural herd immunity. And there are two reasons the situation would likely be worse than that. The first relates to the question of time. Over what period of time would those additional cases occur. We have had over 7 million confirmed cases and 204 thousand deaths in 7 months (March through September). So will these, say, 35 million cases occur over the next 35 months (almost three years) or over less time? If they happen quicker, will they overwhelm our medical infrastructure, which would increase the likely death rate? (And again, this is at the minimum 50% resistance for herd immunity).
The bottom line is that there is no path to natural herd immunity that is not horrific. And the second reason why it is likely much worse is this – we don’t know yet how long immunity lasts. Right now all we can say is that immunity after infection lasts at least three months. It may last longer, but only time will tell. Part of the uncertainty is that our immune systems react different to different agents. Studies so far are finding that antibodies fade after only about three months following COVID-19. But there is also immune memory in T-cells, even after the antibodies have faded. Early research shows they last longer, but again it takes time to see how long they will last.
Let’s say, for example, that immunity lasts for one year. That’s great if you have a vaccine you can get once a year, but is not good enough if your goal is natural herd immunity. Long before enough of the population would have been exposed, resistance will be fading from the first wave. Even if immunity lasts for several years, it’s possible the pandemic will simply move around the world in waves, returning to regions after natural immunity has faded.
There are still some unknowns here, but counting on natural herd immunity does not seem like a viable option, even under wildly optimistic conditions. We need a viable vaccine, and we need people to accept the vaccine. It seems that only then will this all end.






