Jun 26 2020
Face Mask War
 It’s always disappointing (not surprising, but disappointing) when a purely scientific question unnecessarily becomes a political or social one. Whether or not to wear a face mask during an historic pandemic should be purely a question of risk vs benefit – does it work, and is there any downside? The evidence is clear enough at this point that mask wearing helps reduce the spread of COVID-19. David Gorski recently reviewed the evidence, including a recent meta-analysis, and found:
It’s always disappointing (not surprising, but disappointing) when a purely scientific question unnecessarily becomes a political or social one. Whether or not to wear a face mask during an historic pandemic should be purely a question of risk vs benefit – does it work, and is there any downside? The evidence is clear enough at this point that mask wearing helps reduce the spread of COVID-19. David Gorski recently reviewed the evidence, including a recent meta-analysis, and found:
When it came to masks, an analysis of 29 unadjusted and 10 adjusted studies demonstrated that the use of masks was also associated with a large decrease in transmission, both for N95 masks and for disposable surgical masks or similar reusable 12- to 16-layer cotton masks.
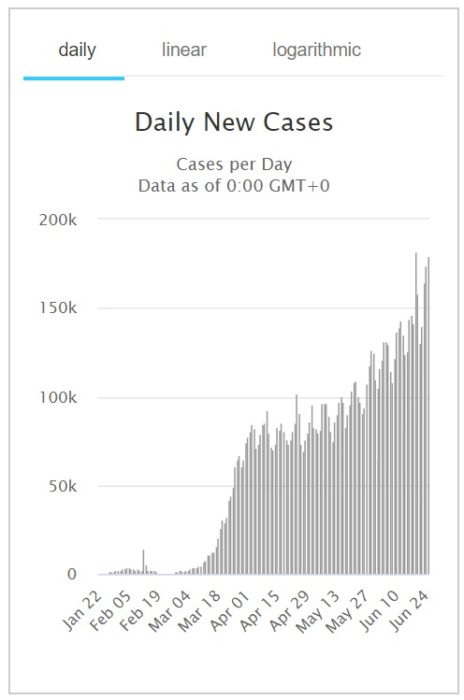
Since that review there have been further studies, such as this one, showing that countries who adopted mask wearing early had fewer cases of illness. The benefit, therefore, seems clear. What’s the downside? Pretty minimal. Sure, it may be a pain and a bit uncomfortable, but this is a minor nuisance at worst. People who are hard of hearing and rely on lip reading probably suffer the biggest downside. There are masks with transparent sections over the mouth to facilitate lip reading, however, for those who need to deal with the hearing impaired.
So wear a mask if you are sick, around other people who are sick, or just in public. In some countries it is considered hygiene etiquette, as it should be.
As a side note, there is some confusion because early on the WHO recommended not to wear a mask in public unless you or others were sick. This was not because the evidence did not support it, however, but because there was a shortage of PPE and people were hording. The idea was to make sure that essential workers had enough masks. This is no longer an issue, and the WHO has revised their recommendations, which are now in line with the CDC – wear a mask, even just to go in public.

 There is
There is  Pangolin’s are adorable and weird animals.
Pangolin’s are adorable and weird animals. The safety and efficacy of hydroxychloroquine for the treatment of COVID-19 has quickly become an important medical question in managing this pandemic, although not by far the most important. There are many drugs under consideration, and some with promising early results. But hydroxychloroquine has garnered the majority of attention for purely political reasons.
The safety and efficacy of hydroxychloroquine for the treatment of COVID-19 has quickly become an important medical question in managing this pandemic, although not by far the most important. There are many drugs under consideration, and some with promising early results. But hydroxychloroquine has garnered the majority of attention for purely political reasons.  A new study
A new study 
 Perhaps one of the positive outcomes of the pandemic is an acceleration of acceptance of telehealth and telementalhealth – treating patients online instead of in person. For example, we have been trying to institute telehealth where I work for years, but have met with roadblocks. Then, all of a sudden, we were able to do it. Our clinic manager estimates that we accomplished in three weeks what would have otherwise taken three years. I have been doing mostly telehealth visits for the last two months now. It’s not perfect, but for many patients it is an ideal option.
Perhaps one of the positive outcomes of the pandemic is an acceleration of acceptance of telehealth and telementalhealth – treating patients online instead of in person. For example, we have been trying to institute telehealth where I work for years, but have met with roadblocks. Then, all of a sudden, we were able to do it. Our clinic manager estimates that we accomplished in three weeks what would have otherwise taken three years. I have been doing mostly telehealth visits for the last two months now. It’s not perfect, but for many patients it is an ideal option.
 As is often pointed out, the SARS-CoV2 virus is new, and therefore we have limited data on its characteristics, as well as the disease it causes, COVID-19. This complicates our modeling of what is likely to happen, and recommendations about best practices. But scientists around the world are busy studying this pandemic as it is occurring, and therefore our models and recommendations are evolving.
As is often pointed out, the SARS-CoV2 virus is new, and therefore we have limited data on its characteristics, as well as the disease it causes, COVID-19. This complicates our modeling of what is likely to happen, and recommendations about best practices. But scientists around the world are busy studying this pandemic as it is occurring, and therefore our models and recommendations are evolving.





