Aug 23 2016
Deaths in Alternative Cancer Clinic Investigated
 Imagine you or a loved-one has cancer. You have a choice between two treatment options. You can be treated by a physician who is a cancer specialist using therapies that have been extensively researched, where we know the risks vs benefit, we know how to dose the treatments, and how to monitor for and manage potential side effect.
Imagine you or a loved-one has cancer. You have a choice between two treatment options. You can be treated by a physician who is a cancer specialist using therapies that have been extensively researched, where we know the risks vs benefit, we know how to dose the treatments, and how to monitor for and manage potential side effect.
On the other hand you can be treated by someone who is not a physician (let alone a cancer specialist), who will also use powerful chemotherapeutic agents, but ones that have not been adequately studied, reviewed, or approved. We don’t know how to safely dose them, what all the possible risks are, or even if the agents work for your type of cancer (or at all, for that matter).
Which would you chose? It is hard for me to imagine why someone would choose the latter. Yet, if you slap the word “alternative” in front of the name of the latter clinic some people will think that it magically makes it the better choice. Also, some people have been so confused by conspiracy narratives they think that the con artist who isn’t a doctor is more trustworthy than the person who has dedicated their life to treating cancer.
Amazingly, they will argue that they don’t trust the doctors because there is too much money in cancer treatment, and then go to a clinic that will charge them $11,000 for unproven therapy.
Deaths at a German Clinic
The most recent example (allegedly, as this is still under investigation) of this phenomenon is a German clinic in Brueggen-Bracht that has been apparently treating cancer patients with an experimental compound called 3-Bromopyruvate. German prosecutors are investigating three recent deaths of patients at this clinic. Following the reports of these deaths, about 70 other families have come forward to report deaths of loved-ones treated at the clinic.
Klaus Ross, a medical appliance seller and technician, ran the clinic. He was schooled as an alternative biological doctor and recruited patients who were told conventional medicine wouldn’t help them beat cancer. Ross also had a license to administer injections and intravenous therapy, CEN reported.
In the US nurses can be licensed to administer IV therapy and injections, but that does not mean they can prescribe the treatments. That still requires a doctor or someone with prescribing authority. I am not as familiar with the regulations in Germany, but it sounds like Ross did not have the authority to prescribe chemotherapy, but was licensed to technically administer IV therapy.
There are many possible risks to this situation. Cancer patients are often very sick. They require careful monitoring and often require treatment for the many possible complications of the cancer itself and also the treatments that are given for the cancer.
Proper management often requires a hospital setting, or at least a clinic that is set up to handle sick cancer patients. Doctors and staff need to be experienced specifically with cancer treatment.
Further, a recent study in JAMA Oncology showed that patients who were using CAM treatments for their cancer were 87% less likely to also receive the recommended standard treatment for their cancer.
3-Bromopyruvate
What about the drug that was allegedly used at this clinic? This is a genuinely promising new chemotherapeutic agent.
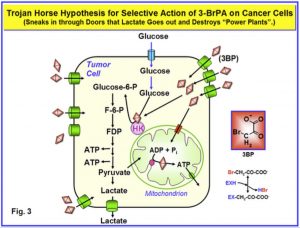
3-Bromopyruvate (3BP) is a new, promising anticancer alkylating agent with several notable functions. In addition to inhibiting key glycolysis enzymes including hexokinase II and lactate dehydrogenase (LDH), 3BP also selectively inhibits mitochondrial oxidative phosphorylation, angiogenesis, and energy production in cancer cells. Moreover, 3BP induces hydrogen peroxide generation in cancer cells (oxidative stress effect) and competes with the LDH substrates pyruvate and lactate.
Chemotherapy in general works by targeting cancer cells more than healthy cells. The drugs are very toxic, they are meant to be toxic, as their purpose is to kill cells. Some traditional agents target rapidly dividing cells, which aggressive cancer cells are. They also target rapidly dividing healthy cells, which is why chemotherapy patients often lose their hair.
Researchers have been looking for newer agents which are more specific to cancer cells by targeting their alternate metabolism. Cancer cells, for example, often thrive in low oxygen conditions by using alternate pathways to produce energy. 3-Bromopyruvate works this way, targeting energy production in some cancer cells.
Still, any drug has potential side effects, and even a chemotherapy drug that is highly selective to cancer cells is likely to have toxic side effects. Further, since the goal of chemotherapy is to kill as many cancer cells as possible, the dose is often pushed as high as can be safely tolerated.
The primary question for research into potential new chemotherapy agents is whether or not there is a dose range that has sufficient activity against cancer cells with tolerable side effects. Many agents that look wonderful in the Petri dish fail in clinical trials because they don’t have such a therapeutic window.
There are also other possible ways for a promising agent to fail. The drug may not get to the cancer cells in sufficient concentration. Cancer cells may also have a way to rescue themselves from the potential toxicity of the agent.
There are so many variables, that no matter how promising a new drug, we need clinical research in actual people to see what the net effects of the drug are. We also need clinical studies to know exactly how to dose the drug and what side effects need to be managed.
So far there are not many clinical trials with 3-Bromopyruvate. One paper looking at a single case found that the drug did not work in a patient with metastatic melanoma. However, another single case report in a patient with fibrolamellar hepatocellular carcinoma showed a good result (although other drugs were also used). That is pretty much it for human trials.
A 2016 review concluded simply that actual clinical trials are needed to confirm the anti-cancer effectiveness of the drug.
It does seem likely that 3-Bromopyruvate will become part of the anti-cancer tool kit in the future. Perhaps we will need to tweak the molecule, or it will have to be combined with other treatments (as some studies indicate), and we still need to find the optimal dosing schedule for specific cancers and stages.
Administering the drug right now, however, outside the context of a clinical trial with proper ethical oversight and informed consent is grossly unethical. Calling it “alternative” does not change this.
This is a great example of what “alternative medicine” is in practice. Forget all the flowery propaganda – so-called “alternative” medicine is simply medicine that has not been adequately researched, is highly implausible, and/or has already been shown not to work.
In this case it is simply a chemotherapeutic drug that has not yet been adequately researched. What is “alternative ” about 3-Bromopyruvate? It is a drug developed from research into cancer cell metabolism. It is a manifestation of the best of reductionist science, translated into a potential treatment.
“Alternative” also means “No standard of care.” That is what we have here. We have someone who is not a qualified doctor or oncologist prescribing and administering an unapproved drug without adequate oversight or ethical controls. There is no question that if this were being done by a regular doctor not hiding behind the shield of the “alternative” label, they would be guilty of malpractice for falling well below the standard of care.
There is no malpractice in the alternative world, however, because there is no standard of care. Anything goes.
If history is any indication, it actually takes dozens of people dropping dead to get the attention of regulators. If investigation confirms what is suspected in this case, and many of the 70 possible victims died as a result of toxicity and improper management, then some legal action may be taken. It is unfortunate that this is what it takes, being the proximal cause of death in many cases.
Being a remote or secondary cause of death is apparently not enough. Your patients can die by the dozens from lack of standard therapy, and that is not enough to shut you down. Simply ripping off your marks (I mean “patients”) for tens of thousands of dollars is also apparently not enough.
Conclusion
We will have to wait for the official investigation to see what was happening at Ross’s clinic, and I will hold my final judgement until then. However, if he were prescribing 3-Bromopyruvate to cancer patients, then in my opinion he should be convicted at the very least of practicing medicine without a license. If the treatment contributed to the deaths of any patients, then he is guilty in my opinion of manslaughter at least.
Meanwhile, the jury is still out on 3-Bromopyruvate. I hope this turns into an effective anti-cancer agent, and the science so far looks very promising. We will have to wait for clinical trials to see how it works out.






