Mar 09 2017
Alzheimer’s and Stem Cells
 A recent article in The Mercury News reports on the work of a neurosurgeon who is injecting fat-derived stem cells into the brains of Alzheimer’s patients. The reports is, unfortunately, typical. It revolves around a heart-wrenching anecdote, while giving the facts with the usual false balance.
A recent article in The Mercury News reports on the work of a neurosurgeon who is injecting fat-derived stem cells into the brains of Alzheimer’s patients. The reports is, unfortunately, typical. It revolves around a heart-wrenching anecdote, while giving the facts with the usual false balance.
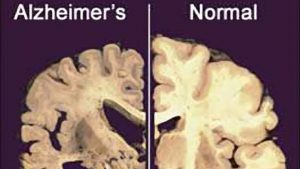
This is the perfect storm for dubious treatments – Alzheimer’s disease (AD) is a progressive dementia that causes sufferers to slowly lose their memories and ability to think. It is a growing problem with our aging population. There are some modest symptomatic treatments for AD but nothing which alters the course of the disease, or can stop or reverse it.
There is no doubt that the need for an effective treatment is great, but that does not justify lower the standards of science in medicine. If anything it means we have to be more careful.
Added to this is the hype and allure of stem cells, which are progenitor cells that can turn into specific cell types. The general idea with stem cell therapy is that the stem cells will replace damaged or dying cells, repair organs, and reverse disease. This is tricky technology, however, and as is common the hype is running ahead of the science. That is a recipe for exploitation and quackery. Fake stem cell clinics have popped up around the world, promising cures but just robbing the desperate of their remaining health and large amounts of money.
Stem cell medicine is legitimate science but needs to be researched properly. It is not easy to get stem cells to do what we want. They may not develop into the kind of cell we need, or “take up shop” and start functioning. They may not survive long, or they may just turn into tumors. The science is progressing, but we are a long way from stem cells as a panacea.
The Mercury News article focuses on neurosurgeon, Christopher Duma. He is taking fat cells from patients, deriving stem cells from the fat, and then injecting them unaltered into the brains of Alzheimer’s patients. This is a very crude use of stem cells. They are not neuronal stem cells, destined to become brain tissue. It seems highly implausible that just dumping fat stem cells into the brain will accomplish anything useful, let alone reverse the brain-wide degeneration of AD.
If Duma thinks he is onto something, or just wants to try a hail-Mary pass for a desperate disease, then the proper thing to do would be to start with animal studies. Do some plausibility testing. Yes, it takes time, but the time is well-invested. Yes it takes money and resources, but you get those resources by convincing someone that you have a scientifically sound idea.
Duma, according to the article, tried to get IRB approval for a study without animal testing but was denied. Another lab did rat testing for him, to test for safety, and this did earn him IRB approval for a Phase I study. These are generally feasibility and safety studies but not efficacy trials. He did not have funding for the study, however. He apparently charged Jack Sage (the patient featured in the article) $10,000 each for eight treatments of stem cells as part of the Phase I study (not covered by insurance). It is generally considered unethical to charge a patient for an experimental treatment.
The News article spends a lot of time recounting how well Sage is doing. His memory and function are improving, which should not happen with AD. They make passing reference to the placebo effect, but that does not seem to explain the improvement they are describing.
The article makes passing mention of this:
Shankle, a renowned expert in cognitive disease – he is the author of the Memory Performance Index that is used around the world – diagnosed Sage with two problems: Alzheimer’s disease and hydrocephalus (fluid on the brain). Sage needed a shunt in his brain to drain the fluid and relieve the pressure.
So Sage received a shunt to treat the hydrocephalus in addition to the stem cells injections. You see the obvious problem here? How do we know that the alleged improvement in Sage is not entirely due to treating the hydrocephalus. Duma says that Sage was a perfect subject, but this would make him a terrible subject. Hydrocephalus can cause dementia, and a shunt can cure the hydrocephalus and reverse the dementia. The article, however, does not point this out or even ask about it, just mentions the shunt in passing.
Conclusion
From the article it seems we have a well-meaning neurosurgeon pursuing a treatment for AD that has some plausibility, but not much. It is more than a bit of wishful thinking to believe that unaltered fat-derived stem cells are going to have any significant clinical effect on AD. If only it were that easy.
But if he thinks there is some potential here I would expect him to be pristine in conducting proper research. This is an invasive procedure, and patients and their families will be desperate. He does hope to get a grant and then he can waive the fee for subjects, but he should have done that for the Phase I study.
The Mercury News article is a huge part of the problem here. The article is designed to give false hope to patients while providing just enough false balance to give plausible deniability.
The bottom line is that a Phase I study is not news for the public. Most treatments at the Phase I level will not pan out. This is the level where treatment ideas should be discussed and debated among researchers and experts. If, for some reason, a science reporter thinks that such preliminary evidence is news-worthy, then you better do a great job putting the evidence and the treatment into context, which they did not do here.






