Jun 03 2021
Return of the Bird Flu
 Remember the bird flu? Avian influenza (H5N1) was first discovered in birds in 1996, with the first human crossover detected in 1997. Since then it has been discovered in 50 countries and is endemic in six. If you are old enough to remember, there was a bit of a bird flu panic back in the late 90s. Fortunately, so far, those fears have not been realized. But it’s important to remember that the bird flu is still around. Even more important is to remember that there are thousands of potentially pandemic viruses in the world.
Remember the bird flu? Avian influenza (H5N1) was first discovered in birds in 1996, with the first human crossover detected in 1997. Since then it has been discovered in 50 countries and is endemic in six. If you are old enough to remember, there was a bit of a bird flu panic back in the late 90s. Fortunately, so far, those fears have not been realized. But it’s important to remember that the bird flu is still around. Even more important is to remember that there are thousands of potentially pandemic viruses in the world.
Avian influenza adapted to infect birds, and mostly spreads through poultry. Bird to human transmission (zoonotic infection) is rare, and usually occurs in those who work in the poultry industry with long term exposure. The virus is very deadly, with a case fatality rate of about 60%. Worldwide there are 700 reported human cases. However, the virus does not spread easily from human to human. Such transmission is very rare, and is not sustainable. This is why the virus has not caused an outbreak or worse among humans. There are also other strains of flu virus that primarily infect birds, such as H10N5. We now have the first report of an H10N5 infection in a human, in a poultry worker in China. Contact tracing did not reveal any other cases.
For now we have experienced rare bird to human zoonotic transmission of flu strains primarily adapted to birds (colloquially “bird flu”) without any significant or sustainable human to human spread. So what’s the concern? As was originally raised by in the 90s, the concern is that every time a virus jumps from an animal reservoir to a human there is the potential that it will either mutate or will combine with another virus to cause a new strain that is highly contagious to humans. It happens, as we are now experiencing with the SARS-CoV-2 virus. So what do we do about it?

 We know a lot more now about SARS-CoV-2 and COVID-19 than we did a year ago when this pandemic was just getting into full swing. One of the big questions was about the emergence of new variants – how fast does the virus mutate, and what is the probability of variants with new properties emerging? Scientists have been tracking the variants since the beginning. It’s actually a good way to track the spread of the virus, and our ability to sequence the genome of specific viruses is fairly advanced.
We know a lot more now about SARS-CoV-2 and COVID-19 than we did a year ago when this pandemic was just getting into full swing. One of the big questions was about the emergence of new variants – how fast does the virus mutate, and what is the probability of variants with new properties emerging? Scientists have been tracking the variants since the beginning. It’s actually a good way to track the spread of the virus, and our ability to sequence the genome of specific viruses is fairly advanced. This was inevitable. We are in the midst of a massive rollout of two new vaccines for COVID-19. Anxiety and fatigue levels from the pandemic are already running high, and there is a pre-existing anti-vaccine movement who is sure to exploit this. But perhaps most significantly, we are now living in a post-social media world. Information, even medical or scientific information, may get to the public unfiltered, ripe to be misinterpreted by people who do not understand the relevant science. Such is the case with
This was inevitable. We are in the midst of a massive rollout of two new vaccines for COVID-19. Anxiety and fatigue levels from the pandemic are already running high, and there is a pre-existing anti-vaccine movement who is sure to exploit this. But perhaps most significantly, we are now living in a post-social media world. Information, even medical or scientific information, may get to the public unfiltered, ripe to be misinterpreted by people who do not understand the relevant science. Such is the case with 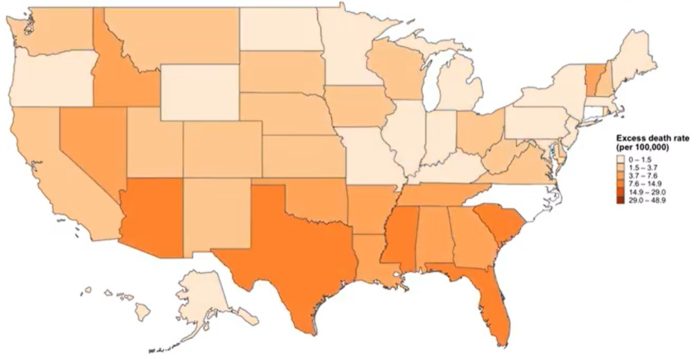 How many people have died in the US so far from the COVID-19 pandemic? It depends on how you count the numbers. The official count of
How many people have died in the US so far from the COVID-19 pandemic? It depends on how you count the numbers. The official count of 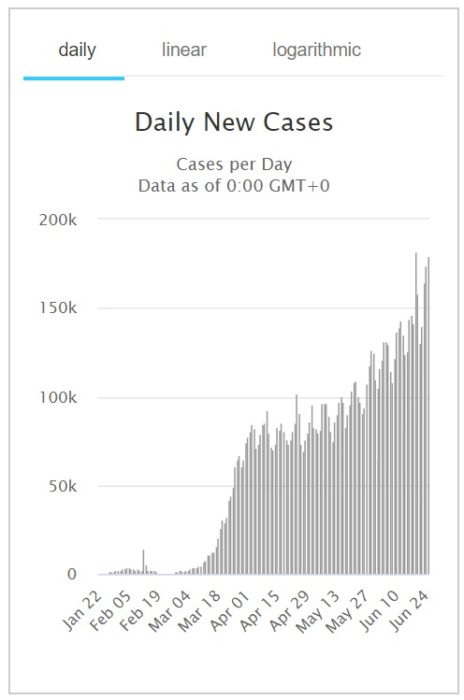 It’s always disappointing (not surprising, but disappointing) when a purely scientific question unnecessarily becomes a political or social one. Whether or not to wear a face mask during an historic pandemic should be purely a question of risk vs benefit – does it work, and is there any downside? The evidence is clear enough at this point that mask wearing helps reduce the spread of COVID-19. David Gorski
It’s always disappointing (not surprising, but disappointing) when a purely scientific question unnecessarily becomes a political or social one. Whether or not to wear a face mask during an historic pandemic should be purely a question of risk vs benefit – does it work, and is there any downside? The evidence is clear enough at this point that mask wearing helps reduce the spread of COVID-19. David Gorski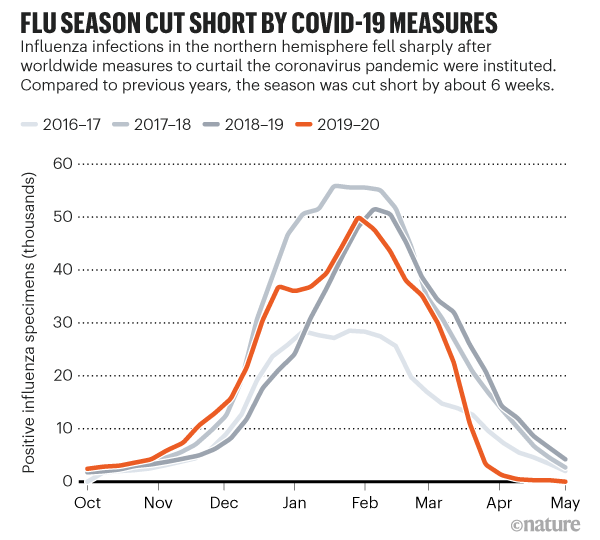 There is
There is 
 It’s important to properly calibrate your concern over new potential threats. Fear is an adaptive trait that focuses our attention and energy on avoiding danger. Too little fear, and we walk into avoidable risk; too much, and we waste time and energy without reason, perhaps even causing unnecessary harm. Proper calibration requires an objective, factual, and balanced approach. Keep that in mind when reading stories and fearmongering about the new Wuhan Coronavirus.
It’s important to properly calibrate your concern over new potential threats. Fear is an adaptive trait that focuses our attention and energy on avoiding danger. Too little fear, and we walk into avoidable risk; too much, and we waste time and energy without reason, perhaps even causing unnecessary harm. Proper calibration requires an objective, factual, and balanced approach. Keep that in mind when reading stories and fearmongering about the new Wuhan Coronavirus. This is going to be a long struggle, perhaps endless. Antivaxxers have been around since there have been vaccines, for over two hundred years, so there is no reason to expect they are going anywhere. Rather, we need an equally permanent anti-antivaxxer movement (otherwise known as the skeptical movement).
This is going to be a long struggle, perhaps endless. Antivaxxers have been around since there have been vaccines, for over two hundred years, so there is no reason to expect they are going anywhere. Rather, we need an equally permanent anti-antivaxxer movement (otherwise known as the skeptical movement).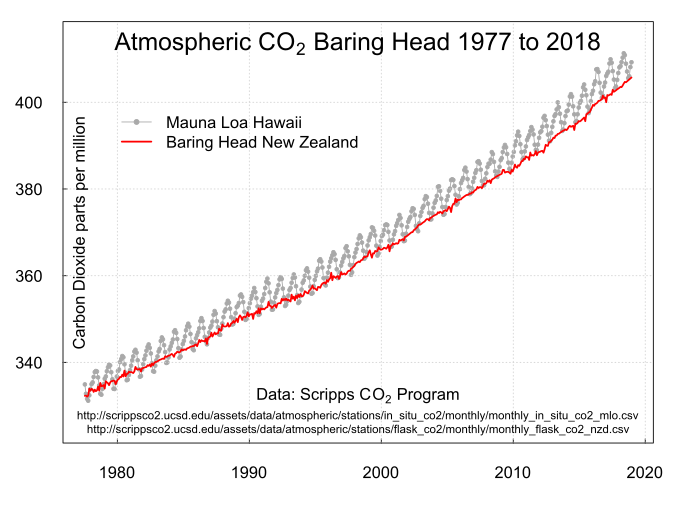 It’s fun and interesting to look back over the last decade and think about what has happened and how far we have come. Round years are arbitrary, but it’s a sufficient trigger to take stock and hopefully gain some perspective on the medium course of history. There is a lot to say about the 2010s, and I may take the opportunity to say more, but I want to discuss in this essay what is perhaps our greatest challenge and disappointment over the last decade. In many ways this has been a lost decade for climate change mitigation.
It’s fun and interesting to look back over the last decade and think about what has happened and how far we have come. Round years are arbitrary, but it’s a sufficient trigger to take stock and hopefully gain some perspective on the medium course of history. There is a lot to say about the 2010s, and I may take the opportunity to say more, but I want to discuss in this essay what is perhaps our greatest challenge and disappointment over the last decade. In many ways this has been a lost decade for climate change mitigation.




