Aug 18 2023
Localizing Hidden Consciousness
 What’s going on in the minds of people who appear to be comatose? This has been an enduring neurological question from the beginning of neurology as a discipline. Recent technological advances have completely changed the game in terms of evaluating comatose patients, and now a recent study takes our understanding one step further by teasing apart how different systems in the brain contribute to conscious responsiveness.
What’s going on in the minds of people who appear to be comatose? This has been an enduring neurological question from the beginning of neurology as a discipline. Recent technological advances have completely changed the game in terms of evaluating comatose patients, and now a recent study takes our understanding one step further by teasing apart how different systems in the brain contribute to conscious responsiveness.
This has been a story I have been following closely for years, both as a practicing neurologist and science communicator. For background, when evaluating patients who have a reduced ability to execute aspects of the neurological exam, there is an important question to address in terms of interpretation – are they not able to perform a given task because of a focal deficit directly affecting that task, are they generally cognitively impaired or have decreased level of conscious awareness, or are other focal deficits getting in the way of carrying out the task? For example, if I ask a patient to raise their right arm and they don’t, is that because they have right arm weakness, because they are not awake enough to process the command, or because they are deaf? Perhaps they have a frozen shoulder, or they are just tired of being examined. We have to be careful in interpreting a failure to respond or carry out a requested action.
One way to deal with this uncertainty is to do a thorough exam. The more different types of examination you do, the better you are able to put each piece into the overall context. But this approach has its limits, especially when dealing with patients who have a severe impairment of consciousness, which gets us to the context of this latest study. For further background, there are different levels of impaired consciousness, but we are talking here about two in particular. A persistent vegetative state is defined as an impairment of consciousness in which the person has zero ability to respond to or interact with their environment. If there is any flicker of responsiveness, then we have to upgrade them to a minimally conscious state. The diagnosis of persistent vegetative state, therefore, is partly based on demonstrating the absence of a finding, which means it is only as reliable as the thoroughness with which one has looked. This is why coma specialists will often do an enhanced neurological exam, looking really closely and for a long time for any sign of responsiveness. Doing this picks up a percentage of patients who would otherwise have been diagnosed as persistent vegetative.
In the last 20 years or so, however, we have increasing had new tools to evaluate these patients, most notably EEG brain mapping and functional MRI scanning. These are both functional scans, they look not at brain anatomy but brain function. When we look at patients who clinically are persistent vegetative we have consistently found that a certain percentage of them, something like 20-40% (depending on the patient population and technique used), have signs of consciousness. They might not outwardly respond to the environment, but their brains do. Give them a verbal task and their fMRI responds, and often in a specific way – different tasks give different responses. Essentially technology has increased the sensitivity with which we can detect subtle neurological responses to the environment. This technology has given rise to a new diagnosis – cognitive motor dissociation (CMD), which means there is a disconnect between what’s happening in the brain and outward motor manifestations. The brain is active, but the patient does not move.
CMD is not the same as what we call locked in syndrome. Patients who are locked in are conscious but paralyzed for some reason. A brainstem lesion at a specific level, for example, can essentially paralyze someone below the eyes, but allow them to remain conscious. Severe motor neuron disease or nerve damage can have a similar result. CMD patients, however, are not just paralyzed. They do have an impairment of consciousness, but it is partial. In fact, one of the findings that has been consistently demonstrated with CMD research is that we see CMD almost exclusively in patients who are comatose due to brain trauma or a severe focal process such as bleeding. We essentially never see it in patients who are comatose because of a diffuse process, such as a lack of oxygen to the entire brain. This suggests that they appear comatose because parts of the brain necessary to outwardly demonstrate their consciousness are not functioning, while other parts of the brain that are able to react to the environment are working. But which parts?
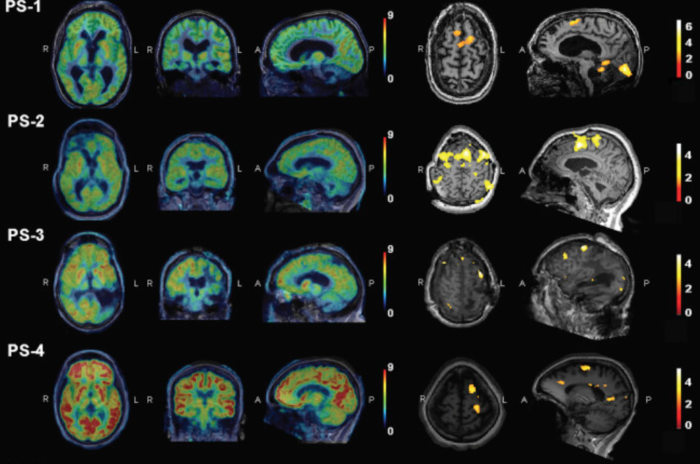
That is the focus of the current study. They looked at CMD and non-CMD comatose patients with both EEG and fMRI scanning to see which networks in the brain were functioning. They found that the patients with CMD (meaning they had some preserved consciousness) with subcortical lesions had greater function in the thalamocortical pathway, while those with bilateral cortical damage had relatively preserved corticocortical pathways than the non-CMD patients. This makes sense, because the thalamocortical pathways are responsible for keeping the brain conscious and awake. Further, consciousness requires a certain minimal amount of the cortex to be functioning and interconnected (about 45%). So in CMD patients these two pathways had to be functioning, while in truly vegetative patients they were not. So what was not working in the CMD patients?
They found that CMD patients had impaired “motor command integration at the anterior forebrain mesocircuit level.” This involved mainly the basal ganglia structures. This part of the brain is not directly involvement with motor function, so again they were not necessarily paralyzed. But this part of the brain is involved with motor planning and intention. Partly it brings together sensory input and conscious input and then feeds that to the motor pathways in order to execute voluntary movement. Essentially with damage to these pathways they are unable to translate the desire to move into motor action. That’s a pretty satisfying result, in terms of fitting in with our current understanding of brain function.
If confirmed with more data, it seems that CMD is largely a result of focal damage to motor command integration pathways. But at this point a question usually arises – does any of this matter to the patient? The short answer is yes, because patients who are in a truly persistent vegetative state have essentially a zero probability of meaningful neurological recovery. This is helpful information to families having to make difficult decisions about goals of care. While patients with a minimally conscious state, including CMD, have a non-zero probability of meaningful recovery. It’s unlikely in the extreme they will go back to anything close to normal neurological function, but they may regain enough function to interact with loved-ones and participate in their care and activities of daily living.
Further, the ability to objectively diagnose CMD based upon signatures of brain function is extremely useful to further research. Being able to objectively define a category is always helpful. Some of this research involved looking at ways, pharmacologically and with brain-machine implants, to bypass or boost the pathways that are impaired. In other words, if enough of the brain is working to generate consciousness, and the patient is not paralyzed, it is theoretically possible to restore significant function if we can bypass the one critical part of the brain that’s not working. We are already seeing the beginning of research into implanting computer chips into patients with specific types of coma to improve their consciousness. This is entirely plausible technology.
The big picture is this – if someone is comatose because a significant amount of their cortex (the thinking part of the brain) is damaged, then for now there is really nothing we can do. They are gone. But if they are comatose because of subcortical structures that are damaged, while the cortical structures are sufficiently preserved, we can wake them up by bypassing the subcortical damage. This greater understanding of the localization of CMD will help research into this technology. There is still a way to go, but this is encouraging progress.






