May 07 2018
The Waking Dead
 Amid a continuous stream of terrible science news reporting, this one stands out from MSN: ‘Miracle’ Boy Wakes After Parents Sign Organ Donation Papers and Days of Being Brain-Dead. Actually the story is based on a local Fox news report. Everyone involved in these stories should be placed in the journalists penalty box.
Amid a continuous stream of terrible science news reporting, this one stands out from MSN: ‘Miracle’ Boy Wakes After Parents Sign Organ Donation Papers and Days of Being Brain-Dead. Actually the story is based on a local Fox news report. Everyone involved in these stories should be placed in the journalists penalty box.
This is a standard fluff narrative that comes up regularly – the person who wakes unexpectedly from a coma, or better yet, after being declared brain dead. There is a common pattern to the stories – you never get enough details to know what actually happened, but what details you do get do not hang together.
The basic facts of the case are this, 13-year-old Trenton McKinley of Mobile Alabama was injured in a dune buggy accident. He suffered severe head injury. Apparently his prognosis was so poor at one point that the doctors talked with his parents about organ donation, and they agreed that if his heart stopped they would go through the organ donation procedure. In other words, they would harvest his organs.
However, before that happened Trenton began to show signs of improvement. He started to move, and then to become conscious. He is now in rehab, able to talk, and to walk with assistance.
While I am very happy for Trenton and his family, this is not an unusual story. Nothing out of the ordinary has occurred here. As far as I can tell (again, from the sketchy details) the only thing that made this even newsworthy was the mother’s misinterpretation of events through the filter of her emotion and religious faith.
To be clear, I hold the mother completely blameless. She went through an unbelievably difficult event, and there is no reason to expect her to understand the nuances of severe brain injury. But that is precisely why the reporters should not have relied upon her interpretation of events for their story. It seems they did so because it created the human-interest narrative they could use. You might notice that no doctors were quoted in the story, or apparently consulted at any stage.
Having been there many times, I can tell you that it may be difficult in some cases to make an accurate prognosis after a serious brain injury. This is especially true when the cause is trauma, and for younger patients. The reason for this is that trauma can cause damage to different parts of the brain, resulting in what we call focal deficits – specific neurological injuries, like the inability to move. But other parts of the brain may be relatively uninjured.
This is distinguished from a diffuse injury, where the entire brain is injured, from lack of oxygen, for example. This can still be tricky to confidently prognosticate early on, but is easier than trauma. Trenton apparently had direct head trauma, but then his heart stopped and he was resuscitated for 15 minutes, so his brain also suffered a relative lack of oxygen.
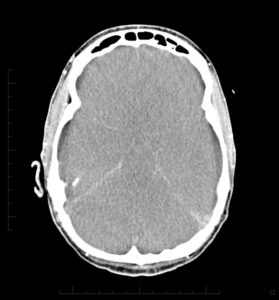
We use various methods to evaluate brain function. The neurological exam is one, and is perhaps the best overall guide. We can also look at the electrical activity of the brain with EEG. Imaging studies look at the anatomy of the brain and may directly visualize the injury. And we can look at blood flow to the brain to see which parts of the brain are viable.
One complication is that after an injury, the brain swells. The swelling is severe enough that it can limit brain function and even cause its own damage. The swelling peaks at about three days, and then slowly reduces. So, we can’t really assess the brain’s potential until the swelling has passed. However, if the swelling gets bad enough it can become fatal in its own right.
Generally speaking, especially in a young patient, we would treat aggressively until after the swelling phase is over, to get a better handle on the long term damage and the potential for recovery. If patients survive (especially young patients) this critical phase, they can sometimes make impressive recoveries. But they may also have permanent severe damage. We can’t always predict confidently, and often just have to wait and see.
Reporting on this case also throws the term “brain dead” around rather loosely, based on the mother’s reports. Brain dead has a specific operational meaning in medicine. It means a very specific procedure was carried out, documenting the complete absence of any brain activity. When a person is documented to be brain dead (with certain details determined state-by-state), then that person can be declared legally dead.
This is the part of the story that makes no sense as reported. The mother claims her son was “brain dead” for three days, but they were going to wait until his heart stopped to harvest his organs. If, however, he really was brain dead, they wouldn’t have to wait. That is part of the reason for having a legal definition of brain death, so that you can declare a patient dead and they can become a candidate for organ donation, even if their heart is still working.
Further, it would not be unusual to discuss organ donation prior to death in such cases. That is preferred, because you want to be ready. What likely happened is that the hospital (there is often now a team of specialists who handle this) talked to the family about organ donation in the event Trenton died. This would affect how they handled end-of-life events, to keep the organs viable. But Trenton never died, he recovered instead.
This is a perfectly ordinary sequence of events. There is no reason to invoke “miracles” or consider Trenton “one-in-a-million.”
Also keep in mind that doctors have to prepare families for the range of possible outcomes. We often say, “I don’t have a crystal ball,” or something to that effect. We cannot predict exactly what will happen, just give a range of possibilities, and prepare for that range. This could include preparing for the worst-case-scenario, while still hoping for the best.
It is also important to recognize that patients and their loved-ones often have difficulty processing a lot of complex information during a time when they are extremely emotional and likely overloaded. I am often amazed at the difference between what I carefully explain to patients, and what they hear.
Basically you cannot trust a second hand non-expert report of a complex medical situation, like the reporters apparently did with this story.
But it made for a sensational headline.






