Jul 19 2011
The Rise and Fall of Placebo Medicine
I am just getting back from The Amazing Meeting (TAM9 from Outer Space) – it was awesome but I had no time to blog while there. One of the events I participated in at TAM was a panel discussion on placebo medicine. We decided to focus on placebos for our science-based medicine panel because it increasingly looks like this will be the front lines for the next phase of the battle against pseudoscience in medicine.
I began the panel discussion by declaring victory, of a sorts. Over the last two decades the public and the scientific community have be told by CAM (complementary and alternative medicine) proponents that we were missing out on many potentially very useful and effective medical treatments simply because they are from other cultures or do not fit into the current scientific paradigm. “Give us the resources to research these diamonds in the rough,” they argued, “and we will give you new tools to promote health.”
Well – a couple a decades and a few billions of dollars worth of research later, and the CAM community has essentially nothing to show for it. The research is in: none of the major CAM modalities actually work. The evidence shows that homeopathy is just water, that acupuncture is no more effective than the kind attention of the practitioner, and that mystical life energies in fact do not exist.
A review of the research funded by the NCCAM, to the tune of over 2 billion dollars, found that all that research has not added one proven modality to the tools of health care. In defending this research the best the NCCAM can do is say that they have demonstrated that some popular herbs do not work, which reduced their market share a bit.
I agree that negative studies of existing treatments are valuable. But the point remains – the research has not gone exactly as the CAM proponents had predicted. Skeptics and more realistic scientists were not surprised that research into highly improbable therapies turned out to have a low probability of finding any of them effective.
What we are seeing now is a transition to the next strategy. Some CAM proponents (while they have generally not given up on their claims to efficacy) are shifting to the claim that while CAM modalities may not work any better than placebo, the placebo is a powerful treatment in itself. In essence they are advocating for placebo medicine via CAM modalities.
Further they are claiming that we should perhaps stop wasting our time doing efficacy trials (researching whether or not their treatments work – because they know how that turns out) and shift to asking how the placebo works and how it can be integrated into care.
I would argue that we already have a pretty good idea of how effective placebo medicine is. That’s what we had in the pre-scientific medicine era, when the average life expectancy was around 40.
To our delight, right before our panel discussion on placebos a major article on placebo effects was published in the New England Journal of Medicine. David Gorski has written an excellent review at Science-Based Medicine, and so I won’t repeat it here. I will just give you the punch line. Take a look at the following two tables.
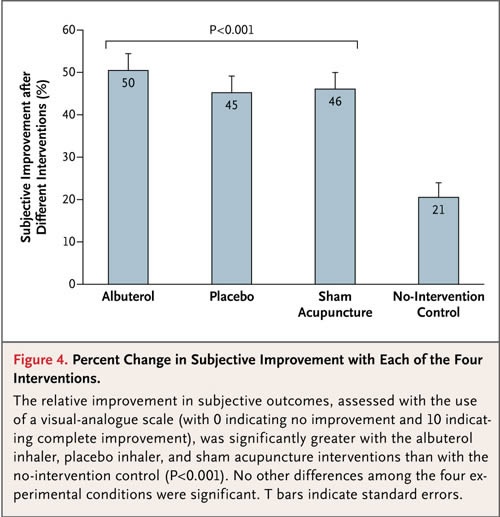
In this study a real treatment for asthma was compared to two placebos, a placebo inhaler and sham acupuncture, and also to a no treatment group. The two charts above give the whole picture. The top figure shows the results for subjective outcomes – how the patient feels. The two placebo groups had an improvement over no treatment, and the real treatment (albuterol) had further improvement.
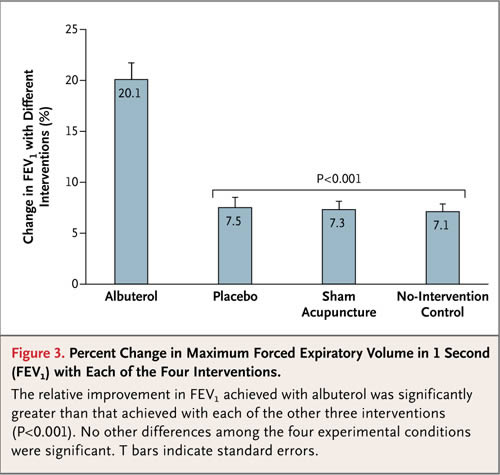
The table below shows the same comparison but for objective outcomes – measuring lung function. Here we see no change from no treatment to either placebo. And again we see an improvement in objective function with the real treatment.
Despite the spin of the authors – these results put placebo medicine into crystal clear perspective, and I think they are generalizable and consistent with other placebo studies. For objective physiological outcomes, there is no significant placebo effect. Placebos are no better than no treatment at all.
It is worth noting that there was still an improvement over baseline, just as there was in the no treatment group. This likely reflects non-specific effects and statistical effects, like regression to the mean. There are many potential effects lumped into the “the” placebo effect that gets measured in the placebo arm of a clinical trial. By comparing to the no treatment group what this study shows is that, for objective outcomes, the placebo effect is entirely made of these non-specific and statistical effects.
This further means that there is no expectation effect or mind-over-matter effect that has a measuring objective physiological effect.
For subjective outcomes (the patient reporting that they feel better) there is a large additional effect. This is likely comprised of reporter bias, expectation, and other psychological effects (which add to the non-specific and statistical effects mentioned above).
What this study strongly suggests is that placebo effects, however, are not real physiological effects worthy of pursuit. They are largely, if not entirely, non-specific therapeutic effect and statistical illusions.
Conclusion
CAM modalities are largely treatments looking for an indication with claims looking for a justification, and now negative research results looking for a rationalization.
The next rhetorical battleground seems to be placebo medicine. Once again CAM-friendly researchers are trying to bolster their position with research, and once again to the extent that technically good research is being done, the results are not supporting their position. And so the spin and marketing begins.
In the end, placebo effects do not appear to be a sufficient justification for any particular treatment ritual. The other conclusion we can draw from the data in this study is that the magnitude of placebo effects for objective outcomes was no greater with a ritual of treatment than with no treatment at all. Further, the magnitude of placebo effects for subjective outcomes was no greater for the elaborate ritual of acupuncture than it was for a simple placebo inhaler.
These results puncture the claim that CAM modalities give a better placebo effect than real medicine.
In other words – any component of the placebo effect worth having you can get from science-based medicine. Pseudoscientific rituals are not necessary – and they come with added risk of promoting pseudoscientific beliefs in health care. As James Randi, who founded TAM, famously said – “It is a very dangerous thing to believe in nonsense.” This is perhaps most true in the field of medicine.






