Jul 29 2022
Wearable Ultrasound Monitor
 It’s easy to take for granted today the revolution in non-invasive medicine over the last century. Prior to the 20th century there was no blood testing to monitor health or diagnose disease. The first clinical use of X-rays was in 1896. The only way to peer into the body prior to that was with auscultation – listening to the sound various organs made, like heart sounds, the lungs breathing, and bowel sounds. Substances that came out of the body could also be examined. A physical examine could sometimes feel what was under the skin, not but deep or beneath bones. There was essentially very little that could be done to non-invasively examine what was happening inside the body. Surgery was the last resort – you had to open up the body and look inside if you needed to see.
It’s easy to take for granted today the revolution in non-invasive medicine over the last century. Prior to the 20th century there was no blood testing to monitor health or diagnose disease. The first clinical use of X-rays was in 1896. The only way to peer into the body prior to that was with auscultation – listening to the sound various organs made, like heart sounds, the lungs breathing, and bowel sounds. Substances that came out of the body could also be examined. A physical examine could sometimes feel what was under the skin, not but deep or beneath bones. There was essentially very little that could be done to non-invasively examine what was happening inside the body. Surgery was the last resort – you had to open up the body and look inside if you needed to see.
Today modern medicine has a long list of options, including using X-rays, magnetic fields, electrical signals, ultrasound, radioisotopes, and tiny cameras to non-invasively or minimally invasively look inside the body. This is all in the last century, a tiny slice of human history. We are also still on the steep part of the curve in terms of increasing our ability to diagnose and treat disease non-invasively. There are frequent incremental advances in the various technologies, and they are adding up over time.
One such incremental advance, which may expand the utility of an entire diagnostic technology, is wearable ultrasound. Ultrasound uses high frequency sound which is projected into the body, usually with a small hand-held probe which is pushed against the skin through a conducting gel. These sound waves bounce back and are picked up by the probe, which sends the information to a computer to construct an image. Anyone in a developed nation who has had a child since 1956 when the technology was first developed is likely familiar with this. Ultrasound is safe, minimally invasive, and can provide a wealth of useful data. It can examine more than fetuses, but can also look at heart function with sufficient detail to detect how the valves are working. It can examine blood vessels to look for clots, or to see if they are open and how they react to stimuli. Ultrasound can be used to look at other organs, to detect cysts or tumors, and to examine the lungs.
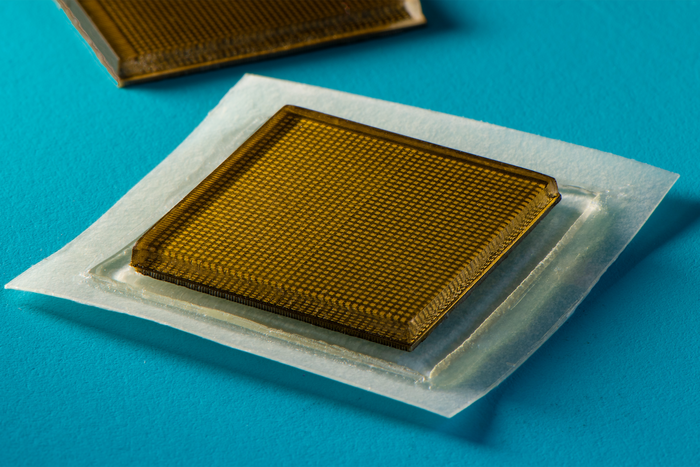
One limitation of the utility of this technology is that it requires a technician to hold the probe in place, which can be tiring and difficult if long term monitoring is desired. Also the conducting gel is necessary to obtain the images, and that gel dries out over time. To solve these limitations MIT scientists have developed sticky ultrasound pads that can be placed on the body and provide long term ultrasound monitoring for up to 48 hours. This approach solves the two problems just mentioned. The pads stick in place and so they can maintain their position relative to the desired body part to be imaged. They also contain an “acoustically transparent hydrogel elastomer” which can last for at least 48 hours.
What about the computer to process the information and create the ultrasound images? This should probably not be hard to guess – you can just use your smartphone. This already exists, small ultrasound probes that can be connected to a smartphone loaded with an app that turns it into an ultrasound machine. This technology isn’t necessary in a modern hospital setting, but is extremely useful in rural, remote, and developing regions. In fact it is part of an effort to build out a suite of medical diagnostic technology that is portable, affordable, and built off a smartphone platform. In essence, with a few attachments, a smartphone can become a modern medical tricorder.
Currently these ultrasound pads would need to be wired to an ultrasound machine, which could either be a dedicated device or an adapted smartphone. This could be worn by the patient, like a Walkman (I hope this reference doesn’t date me too much), and not unlike many portable medical monitors (a Holter monitor for the heart, or a 24 hour EEG monitor). Or a USB-C connection could hook it up to a smartphone. However, the researchers plan on developing wireless technology into the pad, which seems like a no-brainer and should be entirely possible. There are certainly smaller wireless devices. This would then connect to the user’s smartphone, and can communicate in real time to the hospital or office that ordered the monitoring.
What would be the medical utility of this? Doing a one-time test over 20-30 minutes, like a traditional ultrasound, gives a “snapshot” of the anatomy, typically while the patient is lying down. This may be adequate if the medical question is purely about anatomy, or something fixed and unchanging. But if functional information that is likely to fluctuate or change in different conditions is desired, or if transient events are of interest, than long term monitoring is better. For example, an ultrasound pad can be placed over the heart, to look at heart function as a patient goes about a normal day, walking, eating, working, and changing position. Bowel function and blood vessel dynamics could also be monitored in this way.
So while this is an incremental advance in this technology, it does open up the possibility to use it in new ways. This one advance will not “revolutionize medicine”. Such advances are rare. Most are incremental, but they accumulate over time to produce real advance. Also, as a clinician, I can tell you how useful it is to have one more tool in the toolbox. Each specific tool might not be indispensable, but the collection of diagnostic or therapeutic tools is, and each addition makes our jobs and patient outcomes that much better. Each advance chips away at problems that current technology cannot address.
These advances are also inexorably making modern medicine less and less invasive, which improves outcome and reduces pain and distress. We still have a long way to go, but it is amazing to think about how far we have come in just one century.






