Jun 13 2016
Stem Cell Treatment for Multiple Sclerosis
 There has been a lot of reporting about a new stem cell treatment for multiple sclerosis (MS). The results are genuinely interesting, even exciting, but preliminary and need to be put into perspective.
There has been a lot of reporting about a new stem cell treatment for multiple sclerosis (MS). The results are genuinely interesting, even exciting, but preliminary and need to be put into perspective.
MS is an autoimmune disease of the central nervous system, affecting the brain and spinal cord. Actually, it is a category of several diseases that are largely defined clinically, such as relapsing remitting MS and chronic progressive MS. These distinctions are meaningful because they do predict response to certain existing treatments. Relapsing forms of MS tend to respond to chronic immune modulating drugs, while progressive forms tend not to respond.
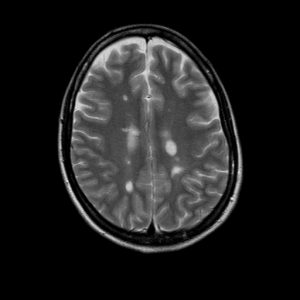
The immune system in MS patients is faulty, targeting the myelin around axons in the brain and spinal cord. Myelin is the insulation that allows axons to conduct. When the myelin breaks down due to inflammation this slows conduction, and if severe enough can even stop it completely. Symptoms depend on where these inflammatory lesions occur in the nervous system. If a motor pathway is affected, then weakness will result.
While the exact cause(s) of MS are not known, the evidence so far suggests that MS is caused by a combination of an inherent problem with the immune system combined with an environmental trigger. Many possible triggers have been implicated, mostly different viral infections. Low vitamin D levels also seems to correlate with risk of MS.
Disease modifying treatments for MS involve immunosuppressive drugs. These target one aspect of the very complicated immune system to reduce the incidence of inflammatory lesions due to MS. Most such lesions don’t cause noticeable neurological symptoms and we track them with MRI scans, while some do cause clinical episodes.
Many MS patients do quite well with current treatments. However, there remains aggressive disease in some patients that respond poorly to treatment.
The Stem Cell Study
The new study looks at relapsing MS patients with aggressive disease not adequately treated by existing drugs. The study is a Phase 2 study, which means there are no controls and it is a relatively small study, with just 24 subjects. The goal of the study was to see if the new treatment is safe and potentially useful, warranting a larger more rigorous study.
The treatment involves using powerful chemotherapeutic agents and specific antibodies to essentially destroy the patient’s immune system. Two days after the final chemotherapy dose, patients are then given autologous haemopoietic stem-cell transplantation (aHSCT). These are immune system stem cells taken from the patient themselves. The transplanted cells then reestablish their immune system.
The idea is to “reboot” the immune system using very young stem cells. Since it can take many years for MS to develop, the hope is that the new immune system will function for many years, and perhaps indefinitely, without the problems that result in MS.
The results of the study are encouraging, but also include reason for caution. Of the 24 subjects, one died of complications of the stem cell transplantation. That is a high risk for any intervention, but of course the small number of subjects does not allow for any confident statistics.
Of the 23 who survived:
Median follow-up was 6·7 years (range 3·9–12·7). The primary outcome, multiple sclerosis activity-free survival at 3 years after transplantation was 69·6% (95% CI 46·6–84·2). With up to 13 years of follow-up after aHSCT, no relapses occurred and no Gd enhancing lesions or new T2 lesions were seen on 314 MRI sequential scans. The rate of brain atrophy decreased to that expected for healthy controls.
So two thirds had essentially no evidence of MS activity for at least three years, and this is without other treatments for MS. One subject had 13 years of follow up without any evidence of MS activity. So, while the treatment is high risk, the outcome is very encouraging. It is possible, even, that this treatment is a functional cure for MS in some patients.
What Next?
These results are encouraging and deserve further research. Such research would include a larger number of subjects and a control group. I doubt the control group would include any kind of placebo. Rather, such a study would randomize subjects to either receive the stem cell treatment or standard therapy. That cannot be double blinded, but you can have doctors examining patients and looking at MRI scans who are blinded to the subject’s treatment status. If there is a dramatic difference in an objective outcome measure, that kind of study design is perfectly adequate.
In addition further studies could start to parse out which MS patients are more likely to respond favorably to such a treatment, and which patients may be at higher risk of an adverse outcome.
There also may be slightly less aggressive interventions with similar outcomes – optimizing risk vs benefit.
This is a serious treatment, but MS can be a very serious disease. That would be a difficult choice, facing a 1/24 chance of short term death for the chance of curing a debilitating disease. Hopefully we can improve those odds, but even still such an option might be worthwhile for patients with very aggressive MS.
I doubt this treatment will become the primary treatment for all MS patients, not with a risk of death that high. It will probably become a desperation treatment for the most severe cases who are not responding to safer interventions. This is not a cure for MS, but another option in a growing arsenal we have to treat this complex set of diseases.






