Jul 23 2020
Herd Immunity and COVID-19
 One of the challenges of dealing with the COVID-19 pandemic, both on an individual patient level and public health level, is that this is a novel virus. We don’t yet have a lot of experience with it or clinical data about how it behaves, what it is capable of doing, and how the immune system deals with it. We are learning fast, but there is still much we don’t know, especially, of course, about long term effects.
One of the challenges of dealing with the COVID-19 pandemic, both on an individual patient level and public health level, is that this is a novel virus. We don’t yet have a lot of experience with it or clinical data about how it behaves, what it is capable of doing, and how the immune system deals with it. We are learning fast, but there is still much we don’t know, especially, of course, about long term effects.
One burning question is – what are the prospects for developing natural herd immunity as the infection spreads throughout communities? Herd immunity (or community immunity) occurs when enough people in a population are resistant to infection due to having effective antibodies that the infection cannot easily spread. This is how epidemics or pandemics burn themselves out – eventually enough people have already been infected and are resistant that the virus cannot find receptive hosts and stops spreading. The percent of the population with resistance needed to achieve herd immunity varies with each type of infection, and can be as high as 90+%. Here are some of the unknowns with COVID-19.
Do people who get infected develop neutralizing antibodies with sufficient activity to resist reinfection?
How severe an illness is required to develop these antibodies? Is a mild or asymptomatic infection enough?
Do these antibodies prevent reinfection alone or do they also prevent passing the virus on to others, even if the host does not get sick themselves?
How long do these antibodies last?
We can add to these questions the variable of a vaccine. For each potential vaccine we need to know what kind and how robust and antibody response is created, does it prevent infection alone or also being a carrier, are booster shots needed, and how long does any resulting immunity last? But until we have one or more vaccines, we are dependent on natural immunity.
Unfortunately (hate to be the barer of bad news) all the preliminary evidence is pointing in the wrong direction with regard to natural immunity. We still need more data, but at this point it does not look like we can pin our hopes on natural herd immunity.
It does seem that patients who are infected, even with a mild infection, do develop antibodies. However, it also appears that the virus can coexist with these antibodies in many patients. There are basically two types of immunity, innate cell-based immunity and adaptive antibody-mediated immunity. What this study shows is that it seems like the innate immunity is more important in clearing the virus than antibody-mediated immunity. This means that you can be infected and clear the infection without having to mount a sufficient antibody response to do it, your innate cellular immunity will take care of it.
Further, the evidence suggests that people with mild or asymptomatic infections do not come away with antibody mediated immunity. What antibodies they form rapidly decay. To further support this, population-based studies in Spain and Sweden show that very few people in the community have antibodies, even in hot spots. Essentially, the idea that because there are large numbers of asymptomatic people with SARS-CoV-2, that this will result in herd immunity and begin to slow the pandemic is probably not true.
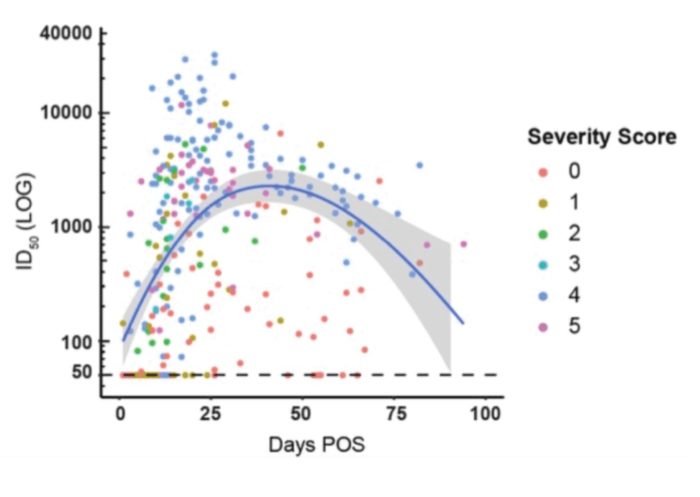
What about people with severe illness? They do develop robust antibody responses, but how long do they last? The news here is not good either.
“Blood tests revealed that while 60% of people marshalled a “potent” antibody response at the height of their battle with the virus, only 17% retained the same potency three months later. Antibody levels fell as much as 23-fold over the period. In some cases, they became undetectable.”
Fading immunity in only several month is really bad news, if this turns out to be true and it holds up with further research. What this would mean is that as the pandemic wave moves around the world, by the time it comes back around immunity will have mostly faded and the pandemic can just keep rolling on. We knew that with the coronavirus family in general immunity does not tend to last very long, but it seems that SARS-CoV-2 is particularly bad in this respect.
So what about a vaccine – will that save us? It remains to be seen. Vaccine immunity may run into the same problems as natural immunity. The advantage of vaccines, however, is that we can at least give a stimulation to the adaptive immune system equivalent to a severe infection. We can also give booster shots timed to maximize antibody response. How long will vaccine immunity have to last for a vaccine program to be practical and effective? Conventional wisdom is at least a year. Longer, of course, is better, but if everyone just has to get their annual shot, that can work. This is partly a matter of limits on manufacturing and distribution. But also, the more frequent the vaccine is necessary, the lower compliance is likely to be. Hopefully, people can just get their COVID-19 shot when they get their annual flu shot.
If any vaccine that is produced lasts less than a year, even if it only lasts a few months, it could still be useful. Healthcare workers and other people in high risk situations could get frequent vaccinations, even if this is not practical for the general population. This would not only protect those at highest risk, it would also shut down locations where the virus is likely to spread, and therefore reduce the pandemic overall. In short – any vaccine is better than no vaccine.
All of this means that we need to be prepared (mentally and practically) for a long battle with this pandemic. Natural herd immunity is likely not going to save us. An effective vaccine might, but also may have limited benefit. Effective treatments are emerging, but they do not generally prevent spread, only reduce the severity of the illness. We are making progress – but this appears to be one nasty virus.






